If you look after an elderly parent, as I do with my mom, you will know that one of the last things you want is to live in a damp house. Our home has a lot of problems with damp, so I invested in a dehumidifier, and it really made a huge difference.
Does Medicare cover dehumidifiers ? Original Medicare does not cover dehumidifiers, as they are “not primarily medical in nature”.
Dehumidifiers reduce the level of humidity in the air, which makes the environment around them less welcoming to dust mites, mold, and mildew – all of which are allergens and can cause irritation to people with respiratory problems or allergies.
I have been using one for over the last two years, and the difference in the air quality is quite marked, and of course you don’t have the unsightly, and unhealthy for some, mold growing in patches in corners.
A dehumidifier draws air in and passes it over cooled elements, which in turn cause the moisture to condense out, and they then pass the air back out over warm elements, so the room doesn’t get cold.
Unfortunately, this is considered to be more of a convenience item by Medicare, and as such can’t be considered for coverage.
Contents Overview & Quicklinks
Does Medicare cover bathroom equipment ?
Does Medicare cover medical supplies?
Does Medicare cover “walking boots” ?
What equipment does Medicare cover ?
How do you get coverage from Original Medicare Part B for DME ?
What is the procedure once you have the signed prescription from your Medicare-enrolled doctor ?
Finding a local Medicare-enrolled DME Supplier near you ?
Does Medicare Advantage cover dehumidifiers ?
List of Durable Medical Equipment typically covered by Medicare
Free one-on-one help with understanding Medicare
Does Medicaid cover dehumidifiers ?
How to find the HCBS programs, waivers and 1915 waivers in your state ?
What’s the procedure for obtaining DME coverage with Medicaid state waivers and HCBS programs ?
Does Medicare cover bathroom equipment ?
Before researching Medicare for my mom, I thought that obvious items such as grab bars, raised toilet seats or shower chairs, or anything making a safer bathroom environment for our elderly parents, would likely get coverage ……
What became clear was that Medicare is not there to help prevent the elderly from having accidents in the home.
Everything which is covered by Medicare must be “medically necessary”, and if you read to the end, you will see this differs greatly from state funding sources, which work to help the elderly maintain their independence in their homes, creating a safe environment for them.
Medicare will not cover any of the following items for bathroom safety –
- grab bars
- raised toilet seats
- bath lifts
- bath seats
- floor to ceiling poles
- shower chairs
- bath chairs
- transfer seats
- toilet safety frames
Medicare does consider equipment for those with serious mobility issues as “medically necessary”, and if you qualify you can get –
- crutches
- walkers
- bedside commodes
all of which can be used in the bathroom as safety equipment.
If you have a Medicare Advantage Plan, you may already be able to have your bathroom safety equipment covered if you are suffering from a chronic illness.
In the fall of 2020 the first Medicare Advantage Plans were allowed to offer new benefits for individuals with chronic illnesses, and among the benefits allowed was some bathroom safety equipment.
Does Medicare cover medical supplies ?
Medicare covers equipment and supplies for use in the home which are durable, and doesn’t typically cover disposable items such as incontinence pads, bandages or gauze, unless the supplies are used in conjunction with a piece of durable medical equipment which they cover.
If you are receiving “Home Health Care” which is covered under Medicare’s Home Health Benefit, some of your supplies would be covered by Medicare Part B.
Does Medicare cover “walking boot” ?
The “walking boot” is the type of equipment that Medicare Part B will cover as Durable Medical Equipment (DME) under the benefit for Orthotics or Braces.
“Walking boot” is a popular form of ankle/foot orthosis.
There are though specific conditions under which Medicare will cover the “walking boot”, or ankle/foot orthosis –
- if the “walking boot” is rigid or semi-rigid – not soft
- if the “walking boot” is being used to immobilize the foot/ankle after orthopedic surgery or for an orthopedic condition
Medicare will not give coverage if the boot is being used to relieve pressure from foot ulcers, as Medicare has therapeutic shoes for people with diabetes, or other conditions which may cause such sores on the feet.
As long as the boot is “medically necessary”, as prescribed by a Medicare-enrolled doctor, you will typically be covered.
What equipment does Medicare cover ?
Durable medical equipment, or DME, is the name of the type of medical equipment to which Medicare Part B extends coverage “for use in the home”.
For Medicare, an item of durable medical equipment has to –
- be able to cope with repeated use over a sustained period of time – durable
- be used for a medical reason only – not just because it is convenient and comfortable
- not easily used by someone who isn’t actually sick or injured
- be principally for use in the home
- be likely to last at least 3 years or more
Typical items of DME are walkers, wheelchairs, crutches, hospital beds, bedside commodes and medical oxygen.
How do you get coverage from Medicare Part B for DME ?
To get coverage from Medicare Part B for DME for “use in the home” –
- you have to be enrolled in Medicare Part B
- have your Medicare-enrolled doctor sign a prescription certifying that the equipment is a “medically necessary”
- you must purchase or rent the DME through a Medicare-enrolled supplier
For Medicare coverage “living at home” is defined as –
- living in your own home
- living in the family home
- living in the community, such as assisted living
What’s the procedure once you have the signed prescription from your Medicare-enrolled doctor ?
You can always ask your doctor, but once you’ve got the prescription –
- you need to see a Medicare-enrolled DME supplier
- you will want to ensure that the supplier is a Medicare-enrolled “participating supplier who accepts “assignment’ – this way you avoid paying any extra
- Medicare gives coverage to the basic models of each type of equipment, so if you want an upgrade you are going to have to pay out of your own pocket, if an upgrade is possible – it isn’t always allowed
- do all the required paperwork with the supplier for your Medicare part B coverage
Assuming that you have used a Medicare-enrolled supplier with your prescription from a Medicare-enrolled doctor certifying that your DME is “medically necessary”, Medicare part B covers 80% of the Medicare-approved price for DME.
If you acquired your DME from a Medicare-enrolled “participating” supplier who accepts assignment, you will only pay your Medicare 20% co-payment of the Medicare-approved price, plus, if it applies, your deductible.
You really must purchase or rent from a Medicare-enrolled “Participating” supplier who accepts “assignment”, otherwise you may pay way more than is necessary.
You should always confirm this with the supplier !
Medicare Rentals – if your item is rented from the supplier you will still have the same payment structure, you will just pay a 20% co-payment of the monthly rental, and your deductible at the outset if it applies.
Finding a local Medicare-enrolled DME Supplier near you
You can use this link to find a Medicare-approved supplier who is local to you – Medicare.gov
What if you have a Medicare Advantage Plan ?
Medicare Advantage plans cover everything that Original Medicare Parts A and B cover, as they are contracted by Medicare to give all the Medicare services.
Advantage plans will also have new extra benefits, but it is pretty doubtful that this covers dehumidifiers, although some are allowing air conditioners for some individuals with chronic respiratory disease.
The procedure for assuring coverage and acquiring the DME will vary according to provider, and each plan will have its own network of doctors and suppliers.
So always contact your plan provider before taking any action, or you may find you don’t have coverage and are left having to pay for everything yourself.
List of durable medical equipment typically covered by Medicare
If you don’t find the equipment you are looking for in my list of Medicare covered DME below, you can use this link to Medicare.gov
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
Free one-on-one help with understanding Medicare
SHIP – State Health Insurance Assistance Programs
All SHIPs offer counseling services to those who need assistance with understanding Medicare, Medicaid and Medigap. Usually it’s conducted over the phone.
Here’s how to find your SHIP contact info – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Does Medicaid cover dehumidifiers ?
Medicaid state programs are funded both federally and on a state level, so as long as they stick within basic guidelines, the states have lots of options to make changes and to adapt programs.
Medicaid can agree to waive particular requirements for eligibility for different programs, which allows a state to provide health care to specific groups of people who might otherwise miss out on getting assistance.
Programs where Medicaid waives requirements are called “waivers” – they will usually have quite specific eligibility requirements, and limited places and often have waiting lists.
This method of Medicaid to drop certain requirements in different cases, has resulted in literally hundreds of different waivers, or programs across the US, all with different eligibility criteria.
Each state has its own range of programs, so do check to see what they offer.
Health Care in the home – Medicaid and state programs
Programs for low income families, the disabled and the elderly which provide health care in the home are called “Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers”.
The programs serve to help the participants to maintain their independence in their homes, and the community.
One aspect of these programs’ work is to cover “home medical equipment”, and frequently the program will cover the costs 100%.
If you want to know if you are eligible for any programs, contact your State Medicaid Agency here.
To discover more on the topic of HCBS programs, or waivers, you can use the link below to medicaid.gov –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
For these Medicaid and state programs the term “home”, for a participant, is used to mean the following –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
Programs and waivers for home care which permit the widest interpretation of DME for coverage
Consumer Direction or Self Direction
Some HCBS programs and waivers employ a system of budget self-management called either “Consumer Direction”, or “Self Direction”.
The participant self-manages how their allocated program budget is spent.
The participant of the program is given a sum of money to cover their needs, and the assistance of an appointed a financial advisor, who is there to guide them.
Medical equipment and other, which is considered essential to their being able to maintain their independence in their homes, as long as the budget covers it, is usually allowed.
The equipment permitted and given coverage as Durable Medical Equipment is a lot wider in range than that with Medicare.
You can find out more about Medicaid Self Direction, click here.
The Medicaid program “Money Follows The Person”
“Money Follows The Person” is a Medicaid program which was set up to assist elderly adults in nursing homes to move back to into their own homes.
The Medicaid program helps with the funding for the different states to build their own Money Follows the Person programs – the state programs can use their current HCBS waivers to assist the elderly in managing their care in their own homes, or it can take the Medicaid funding and design new programs from the ground up.
Each individual elderly case is assessed, and all that is essential to the move, and to maintaining that person’s independence, will be covered by the program.
Programs may give money for remodeling parts of the home to make things safer, improve lighting, build ramps etc., or help buy simple medical equipment such as a shower chair.
As you can see, once again, the range of DME allowed is considerably greater than that which is allowed on Medicare.
How to find the HCBS programs, waivers and 1915 waivers in your state
I have written up a guide of what Medicaid and state HCBS programs and waivers are run in each state for seniors, with links to the different program websites.
You can find it here – “Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”.
What’s the procedure for obtaining DME with Medicaid, state waivers and HCBS programs ?
Step 1
– the doctor, or therapist, has to provide a medical justification letter, stating it is medically necessary
Step 2
– find a Medicaid-approved DME supplier, and give them the medical justification letter
Step 3
– the Medicaid-approved supplier fills out a Prior Approval Application form for Medicaid
Step 4
– the Prior Approval Application is sent to the Medicaid State Office
Step 5
– if you are unsuccessful you will be contacted and given the reasons as to why, as well as advice on how to make an appeal
Step 6
– if approved, you will receive the DME
If your income is a bit too high to qualify for Medicaid
Spend Down Programs
Medicaid’s Spend Down programs are an initiative to help people to get Medicare coverage.
The programs employ several methods to lower a participant’s income level, or income + assets level, by allowing the deduction of certain medical and other expenses.
The goal is to lower the amount of assets and income a participant has, so that it is below the limits of what is allowed for Medicare coverage.
The two methods are –
- Income Spend Down
- Asset Spend Down
I’ve written an article about how it works, which you can find here – What is Spend Down ?
To find your State Medicaid State Agency
If you want to discuss things, or to email someone, you can contact your state Medicaid Agency here.
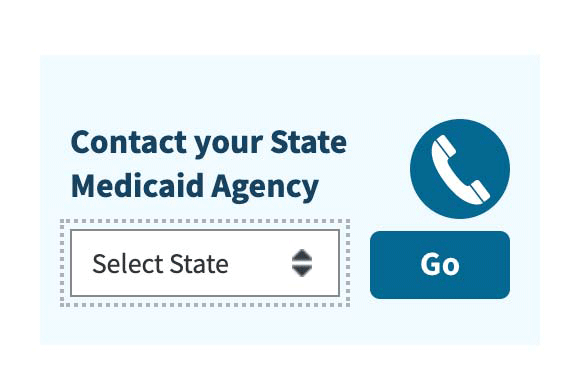
Step 1 –
Click the link to Medicaid.gov and look for the section that I have outlined in red.
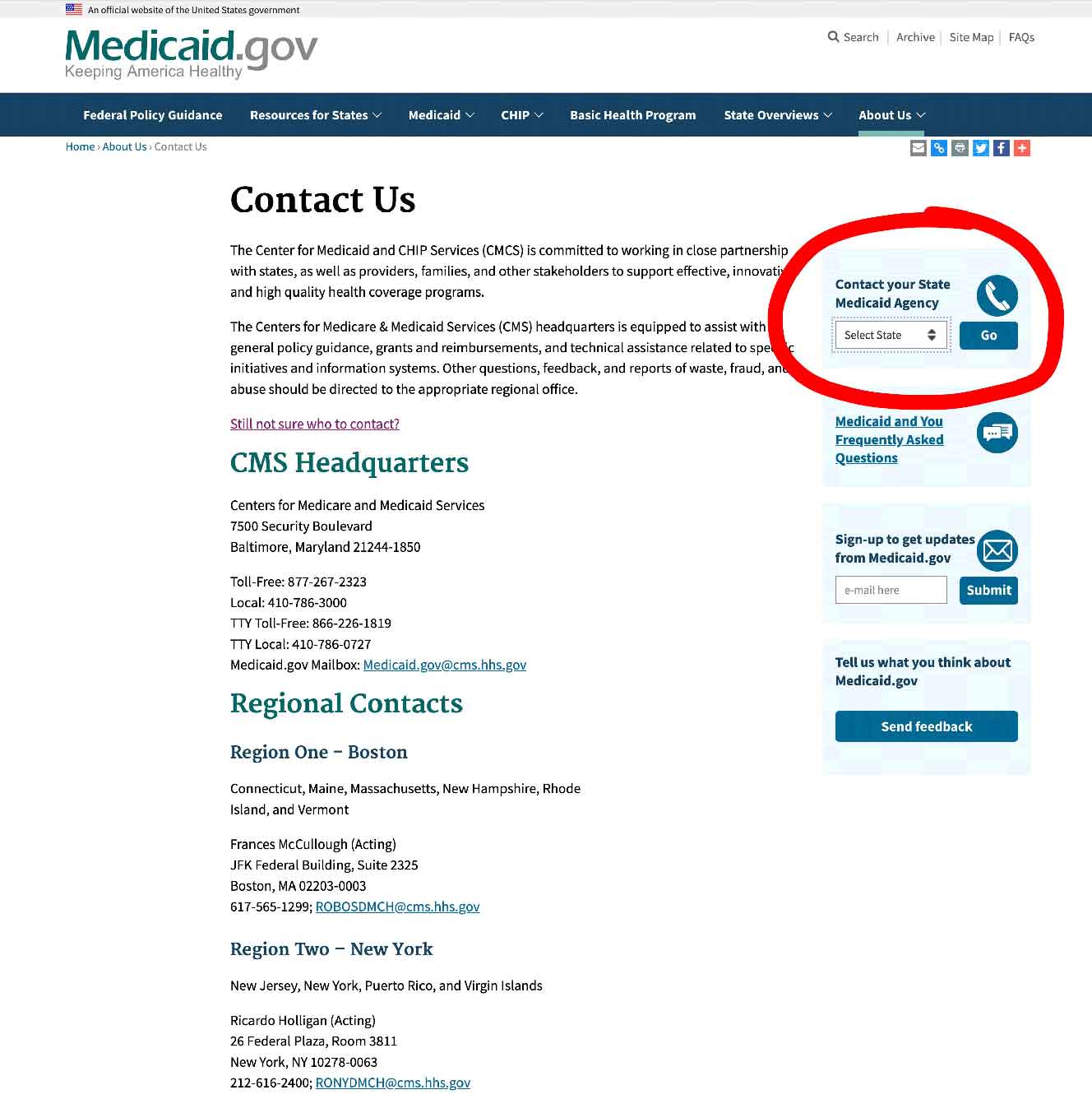
Step 2 –
Select your state and click on the button they have marked “GO” – it will take you to your State Medicaid Agency with all their contact info.
State Funding Assistance
Assistive Technology Programs
Assistive Technology Programs, in all states across the US, have been designed to improve access to assistive devices in the home, primarily for the elderly and the disabled.
Most State Assistive Technology Programs have –
- an online exchange people will post assistive devices and medical equipment for sale, or as donations on a first come, first served, basis – state residents can just register on the exchange website and participate
- a main website where you can make contact and ask about how to get access to free equipment, and what the eligibility requirements are
- reuse and refurbishment programs which are run by the state program, or partnered with community groups, to help them provide free or extremely low cost equipment for the disabled, the elderly and other disadvantaged individuals – sometimes the equipment is free, and in other cases you have to pay a little, depending on the individual’s circumstances
- some states have loan closets as part of their program, and particularly short term loans for checking that the equipment suited to an individual
Assistive Technology Programs will also make contact with individuals who enroll when they know that there is equipment available that the person needs.
You can find out about this on your state assistive technology program website.
To see what projects are in your state, click here.
Step 1/
Pick your state on the map or the drop-down menu, and click on “Go to state”
– I chose Florida for this example
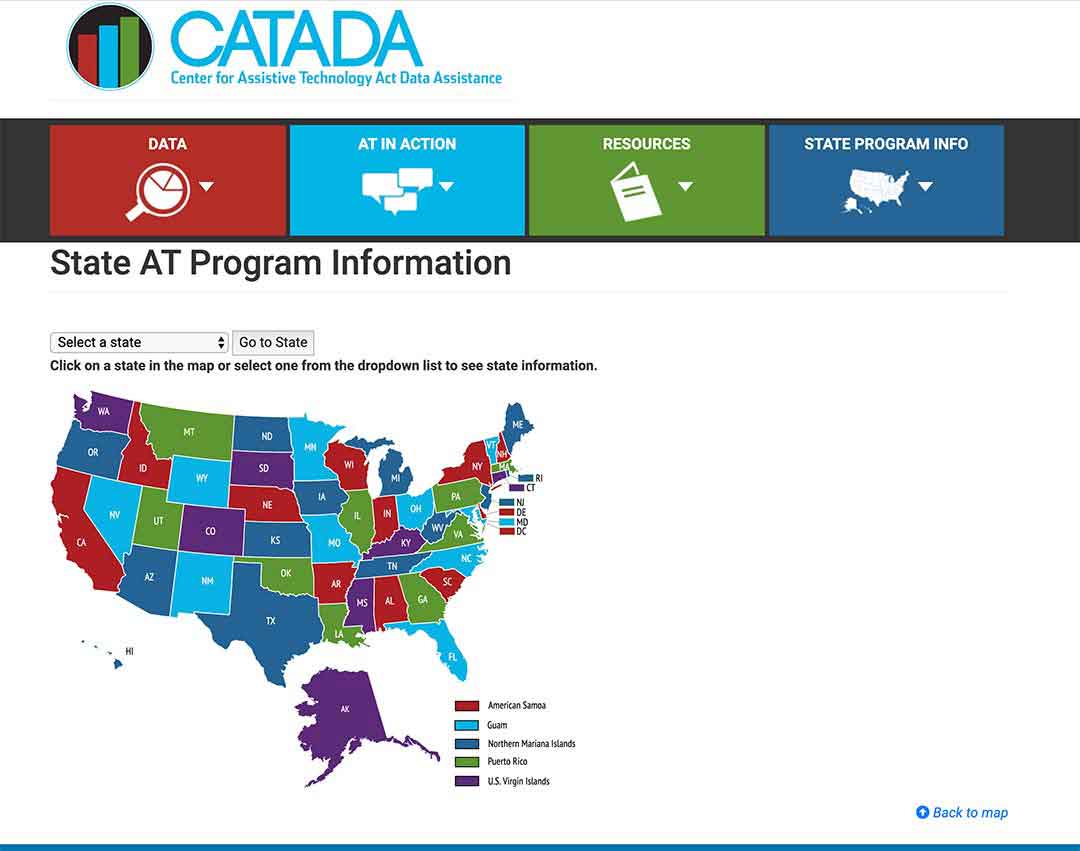
Step 2/
Click on the link “Program Title” – for my example I outlined it in red.
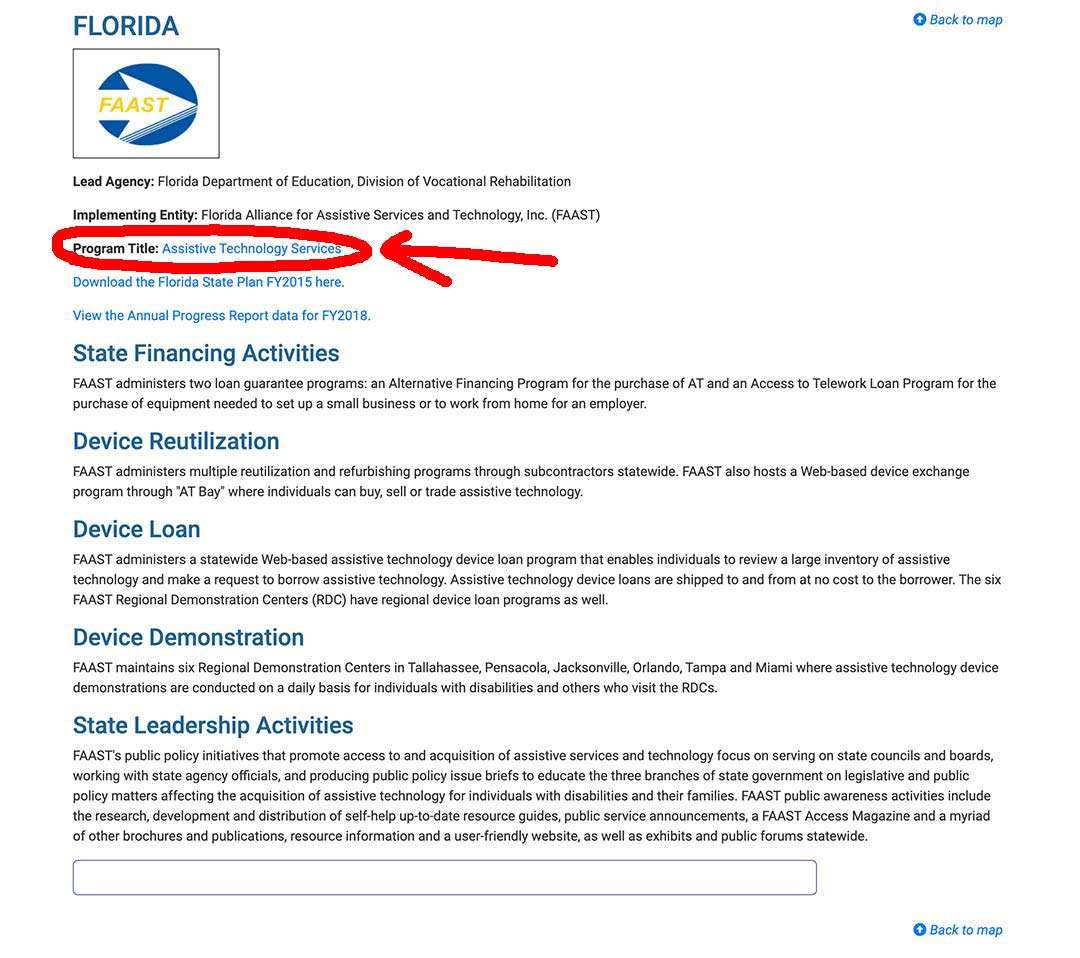
Step 3/
The AT Program state website will come up, and you can sign up, or use their contact info .
State Financial Assistance Programs
Not all, but a number of states, have non-Medicaid programs designed to help the elderly, and the disabled, to remain living independently in their own homes.
State Financial Assistance Programs will pay for assistive and safety equipment, as well as home modifications – remodeling bathrooms, wheelchair ramps, kitchen equipment etc.
The programs pay with grants or loans, or a combination of both.
Your local Area Agency on Aging should be able to tell you more about the financial assistance programs for the elderly in your state.
Summary
You cannot get a dehumidifier with Medicare Part B for use in the home, as it is not considered to be “Durable Medical Equipment” which is the category of equipment for which Medicare offers coverage.
Air purifiers, dehumidifiers, most humidifiers, air conditioners and room heaters are not typically given coverage by Medicare Part B as they are considered comfort items and not medically necessary.
Most bathroom safety equipment falls into the same trap of being considered comfort equipment, although Medicare Part B will cover crutches, walkers and bedside commodes.
With Durable Medical Equipment, Medicare will cover 80% of the Medicare-approved price, as long as you have a prescription from a Medicare-enrolled doctor, and you have used a Medicare-enrolled supplier, and you will typically be responsible for your 20% co-payment and your deductible if it applies.
Always ask the supplier if they are a Medicare -enrolled “Participating” Supplier who accepts “assignment”, as it will limit your financial participation in the purchase.
If you qualify for a Medicaid HCBS waiver or non-Medicaid state program, they, in many cases, accept a broader range of equipment as DME and will often pay 100% of the cost.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.

