Original Medicare does not cover toilet safety frames as they are not considered medically necessary, but Medicare Advantage plans may do so.
Contents Overview & Quicklinks
Medicare Part B does cover bedside commodes
Does Medicare cover shower chairs ?
Does Medicare cover toilet seat risers ?
Does Medicare cover bathroom equipment ?
Do Medicare Advantage plans cover toilet safety frames ?
Will medicare pay for bathroom modifications or remodel?
What equipment does Medicare pay for?
List of durable medical equipment which is typically covered by Medicare if you qualify
Medicare-approved Supplier near you ?
List of durable medical equipment which is typically not covered by Medicare
How do you, or your loved one, qualify for Medicare Part B covered DME ?
What do you, or your loved one, do once you have a prescription for your DME ?
What mistakes do you, or your loved one, need to avoid with Medicare ?
Get free assistance with understanding Medicare
Does Medicaid cover toilet safety frames ?
Medicaid and state programs for care in the home
Programs designed to transition people back from care institutions, into their homes
How to find the HCBS programs, waivers and 1915 waivers in your state ?
What is the path to acquiring DME with Medicaid and state waivers, and HCBS programs ?
If your income is a bit too high to qualify for Medicaid
Medicare Part B does cover bedside commodes
Toilet safety frames are primarily used to assist a person to sit down on, and get up from the toilet safely, by giving them something to hold onto.
A bedside commode is covered by Medicare Part B, and this can be placed over the toilet and used as a toilet safety frame.
The essential difference in why a bedside commode is covered, and why a toilet safety frame is not, is that to qualify for a bedside commode you need to a medical reason, one which is stopping you from using the toilet itself –
- the person is confined to a single room
- the person is confined to one floor of the home environment with no toilet on that level
- the person is confined to the home with no toilet facilities
The reason the person is confined has to be a medical reason, and Medicare will cover the bedside commode for use at the bedside, or wherever else the user chooses to have it.
The bedside commode has to be prescribed, and signed for, by a Medicare-enrolled doctor certifying that it is “medically necessary”, and it has to be bought, or rented, from a Medicare-approved equipment supplier.
Medicare Part B typically covers 80% of the Medicare-approved cost of the equipment, and the beneficiary pays their 20% coinsurance and, if it applies, their deductible.
If you want to learn more about raised toilet seats in all their various types, I have an extensive article which outlines the types and how they fix to the toilet, “Types Of Raised Toilet Seats: What You Should Know Before You Buy”.
For larger individuals who may be worried about the solidity and weight
capacities of the various types of raised toilet seats, I have two articles –
“The Most Secure Raised Toilet Seat ? How To Make The Right Choice ? 50 Plus Examples”
The article covers the types of raised toilet seats and their solidity. In addition, it covers all the types of bedside commodes which you can use over a toilet as a raised toilet seat, with lots of examples of models you can find online, or in the stores. All the models are accompanied by their weight capacity, manufacturer and model number.
“A Complete Beginner’s Guide To Raised Toilet Seats For A Large Person”
This article has 75 examples of raised toilet seats with weight capacities ranging from 250lb all the way up to 1200lb. The difference between the two articles is that this article is specifically for larger individuals, who as well as wanting a strong seat will also probably be wanting a wider seat. All seats have their weight capacity and model number listed alongside the name and manufacturer of the seat.
Does Medicare cover shower chairs ?
Medicare Part B does not cover shower chairs for use in the home, as they are considered to be a comfort item.
As of the fall of 2020, Medicare Advantage plans, which are run by private companies contracted to offer the same services as Medicare, have been allowed to offer some new benefits, and some plans may offer bathroom equipment such as shower chairs
Does Medicare cover toilet seat risers ?
Medicare does not offer coverage with Medicare Part B for toilet risers as, just like with shower chairs, they are considered to be a comfort item and not primarily medical in nature.
As I noted above, you may though be able to find Medicare Advantage plans which are now offering some benefits for bathroom safety equipment.
Does Medicare cover any bathroom equipment ?
I should point out at this point, that although Medicare Part B will not cover a toilet safety frame, among the equipment it will cover, if it is deemed “medically necessary” is a bedside commode.
One type of bedside commode is a 3-in-1 commode, and luckily for us a 3-in-1 commode is so called, as it can be used for three different functions –
- as a bedside commode
- as raised toilet seat
- and as a toilet safety frame
If you can get your doctor to certify that a bedside commode is “medically necessary”, you will be able to use a 3-in-1 commode as a safety frame around your toilet as well.
A few other items that can be used as safety equipment in the bathroom are covered by Original Medicare Part B – walkers, crutches and patient lifts are covered by Medicare Part B, and they can each be used in the bathroom to help with stability and safety.
The reason that Medicare does not cover bath lifts, shower chairs, transfer seats or raised seats for the toilet, as it considers these to be “convenience” or “comfort” items, and not “primarily medical in nature”.
If you, or your loved one, qualify for a patient lift under the Medicare Part B guidelines, you can use that as a bath lift or shower lift.
If you want to find out about the Medicare guidelines for qualification for patient lift coverage, you can find that in either of my articles on Medicare and patient lifts, or Medicare and Hoyer lifts (these are a very popular brand, and the article, as well as explaining the qualification guidelines, also explains which of the Hoyer lifts are covered).
Medicare Advantage Plans are a little different from Medicare Parts A and B, as they are run by private companies under contract with Medicare.
Do Medicare Advantage plans cover toilet safety frames ?
Medicare Advantage Plans are offered by private companies contracted by Medicare to provide Medicare services, and they must, by law, provide at least the same coverage and services, as Original Medicare Parts A and B.
Advantage Plans may also provide more benefits, and some may include bathroom safety equipment not covered by Original Medicare.
Recently Medicare has expanded the benefits that Medicare Advantage may allow, to increase its competitiveness, and some bathroom safety equipment may be allowed to help individuals with chronic conditions.
As to the equipment, it will depend on the plan in question.
If you or a loved one change over to an Advantage Plan, you will have to use the plan provider’s network of doctors and suppliers, so that you do not fall foul of the coverage.
Like Original Medicare Parts A and B, Medicare Advantage plans usually have a co-pay. The rates of the co-pay will be specific to each plan, and to its provider.
Will Medicare pay for bathroom modifications or remodel ?
Original Medicare does not typically cover any bathroom modifications due to the fact that safety equipment and remodeling are not considered to be medical in nature by Medicare.
A lot of safety equipment, as I said above, is considered by Medicare to be “for comfort” and that alone disqualifies it for coverage.
However, as of the fall of 2020, Medicare Advantage plans are being allowed to add new benefits, so that some plans may offer coverage for items of bathroom safety equipment such as grab bars.
I have an article “Will Medicare Pay For Bathroom Modifications ?” with a full explanation of this topic, plus other options for paying for bathroom modifications, or remodeling, with –
- Medicaid – HCBS waivers, 1915 waivers and other programs
- State AT programs – all sorts of free or low cost bathroom equipment
- online exchanges for low cost or free bathroom equipment
- grants for home modifications for the elderly
- State Financial Assistance Plans for grants for the elderly
- USDA grants
- Veterans Direct HCBS
- Low Income Home Energy Assistance Programs
- nonprofits offering their services to help with low cost or free home modifications
You can find that here
What equipment does Medicare pay for ?
Medicare Part B covers some durable medical equipment, or DME, for use in the home.
For durable of equipment to be covered by Medicare Part B you will need, as a minimum, the following –
- a signed prescription certifying that the equipment is “medically necessary”
- the prescription must be from a Medicare-enrolled physician, or treating practitioner
- the equipment must be bought, or rented, from a Medicare-approved supplier
Typical examples of durable medical equipment, which are often sited in Medicare’s own literature, are items such as –
- wheelchairs
- walkers
- crutches
- transport chairs
- bedside commodes
- hospital beds
These are all pieces of equipment which are medical in nature and can withstand repeated use over a sustained period of time.
Medicare won’t cover equipment which is for comfort, and not primarily medical in nature.
Disposable medical equipment and supplies are also not normally covered by Medicare part B.
Examples of disposable supplies which aren’t covered are –
- fabric dressings
- disposable gloves
- bandages
- disposable face masks
There are two exceptions to covering disposable supplies –
- if you are covered for Medicare’s Home Health benefit, some disposable supplies are covered
- if you are covered for a piece of durable medical equipment and a disposable supply is used in conjunction with it, it will typically be covered
For durable medical equipment to be covered by Medicare Part B, it must meet the following criteria:
- Durable (must be able to withstand repeated use overtime)
- It can only be used for a medical reason, as opposed to just for comfort
- Not normally of use to someone who isn’t sick or injured
- You must have it for use in your home
- Should have an expected lifetime of at least 3 years
If your choice of equipment does not meet these basic criteria, you most likely won’t get coverage from Medicare part B.
List of durable medical equipment which is typically covered by Medicare if you qualify
If you don’t find the equipment you are looking for in my list of Medicare covered DME below, you can use this link to Medicare.gov
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Medicare-approved supplier near me ?
To find a local Medicare supplier in your area try this link at Medicare.gov
List of durable medical equipment which is typically not covered by Medicare
Adult Diapers
Air Cleaners
Air Conditioners
Alcohol Swabs
Augmentative Communication Device
Bathroom Aids
Bathtub Lifts
Bathtub Seats
Bed Bath
Bed Boards
Bed Exit Alarms
Bed Sensor Pads
Bed Lifter
Beds – Lounge
Bed Wedges
Blood Glucose Analyzers
Braille Teaching Texts
Caregiver Paging Systems
Catheters – except those which are used for permanent medical conditions where the catheter is considered as a prosthetic
Chair Exit Alarms
Chair Sensor Pads
Communicator
Contact Lenses – Medicare helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens
Dehumidifiers
Dentures
Diathermy Machines
Disposable Bed Protectors
Disposable Sheets
Door Exit Alarms
Easygrip Scissors
Elastic Stockings
Electrical Wound Stimulation
Electrostatic Machines
Elevators
Emesis Basins
Esophageal Dilators
Exercise Machines
Exit Alarm Mat
Eye Glasses – Medicare helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens.
Fall Alarms
Fans
Fabric Supports
Fomentation Device
Grab Bars
Grabbers
Gauze
Hearing Aids
Heat and Massage Foam Cushion Pad
Heating and Cooling Plants
Home Modifications
Humidifiers – not room humidifiers
Incontinence Pads
Injectors (hypodermic jet pressure powered devices for Insulin injection)
Irrigating Kits
Insulin Pens
Massage Equipment
Motion Sensors
Motion Sensor Exit Systems with Pagers
Needles
Oscillating Beds
Over bed Tables
Paraffin Bath Units (if not Portable)
Parallel Bars
Portable Room Heaters
Portable Whirlpool Pumps
Preset Portable Oxygen Units
Pressure Leotards
Pressure Stockings
Pulse Tachometer
Pull String Alarms
Raised Toilet Seats
Ramps
Reading Machines
Reflectance Colorimeters
Sauna Baths
Special TV Close Caption
Speech Teaching Machines
Stair Lifts
Standing Table
Support Hose
Surgical Face Masks
Surgical Leggings
Syringes
Telephone Alert Systems
Television Assistive Listening Devices
Telephone Arms
Toilet Seats
Treadmill Exercisers
Walk in Bathtubs
Wheelchair Lifts
Whirlpool Pumps
White Canes
Wigs
How do you, or your loved one, qualify for Medicare covered DME ?
For durable medical equipment that you need for use in your home, to qualify for Medicare coverage, you must –
- be enrolled in Medicare Part B
- have a prescription signed by your Medicare enrolled doctor saying that the equipment is a medically necessary
- purchase the DME from a Medicare-enrolled supplier
Care facilities – hospitals, or nursing homes, don’t qualify as a “home” for Medicare Part B, although a long-term care facility, such as assisted living can qualify as a “home” for Medicare part B.
Care facilities, as defined above, are covered under Medicare Part A (hospital treatment) and any DME needed when in a nursing facility for up to 100 days should be covered by the facility.
Original Medicare part B defines living at home as –
- living in your own home
- living in the family home
- living in the community, such as assisted living
What do you, or your loved one, do once you have a prescription for your equipment ?
Once you have a prescription from a Medicare-enrolled doctor, Medicare will typically pay for 80% of the Medicare-approved price of your loved one’s DME.
This leaves your loved one responsible for their Medicare co-payment which is equal to 20% of the Medicare-approved price of the DME, and only if they have used a Medicare-enrolled “participating” supplier who accepts assignment.
If not they may much more may be more – so read on !
Your loved one will also have to pay their annual deductible (if it hasn’t already been met).
For less expensive items, Medicare will usually purchase them outright, and for more important purchases they will rent the items on a monthly basis from the supplier.
If the equipment is rented from a Medicare-enrolled “participating” supplier who accepts assignment, your loved one will pay a monthly co-payment of 20% of the Medicare-approved rental price, and their deductible if it applies.
What mistakes do you, or your loved one, need to avoid with Medicare ?
To pay the least amount possible for any equipment, your loved one has to use a Medicare enrolled “participating” supplier who accepts “assignment”.
This ensures the item is being purchased for the lowest possible price – the Medicare-approved price.
Why is this ?
Medicare-enrolled suppliers divide into two groups –
- Medicare Suppliers
or
- Medicare “Participating” Suppliers
Medicare “Participating” Suppliers have an agreement with Medicare to accept what is called “assignment” – they can only charge the Medicare-approved price for DME.
Non-participating suppliers have not come to this agreement with Medicare and can charge 13% extra on the Medicare-approved price, and your loved one will be footing the bill for the extra.
Get free assistance with understanding Medicare
SHIP – State Health Insurance Assistance Programs –
SHIPs offer free counseling services, generally over the phone, for help with Medicare, Medicaid and Medigap from their state program.
I have a very quick article explaining how to locate your SHIP, which you can find read here – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Does Medicaid cover toilet safety frames ?
Funding for Medicaid programs is done both at a federal and a state level.
A state may have any number of different Medicaid programs and waivers, and each with different eligibility guidelines, resulting in hundreds of programs for Medicaid throughout the US.
Medicaid in skilled nursing facilities and hospitals
In hospitals and skilled nursing facilities, the job of ordering the equipment needed for your loved ones will be handled by the facility.
Medicaid and state programs for care in the home
Medicaid programs which are for outside skilled nursing facilities go under the labels of “Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers”.
The programs and waivers are there to help the participants to maintain their independence in their own homes.
A comprehensive explanation of HCBS programs and waivers with more technical information is available at this link to medicaid.gov –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
The programs and waivers for the home, like Medicare, pay for “home medical equipment”, but unlike Medicare, will often cover 100% of the cost of the equipment.
For “Waivers” and HCBS, the term “home” is used to mean that the beneficiary must be living in –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
Coverage of DME, for the home, may be easier to obtain with certain Medicaid waivers, than with others
Certain HCBS programs and waivers allow for what is called Consumer Direction/ Self Direction.
A participant in a program which has “consumer”, or “self direction”, will have an allotted budget to cover their needs, and to help them maintain their independence.
The participant has a financial planner appointed to them to help manage the funds to meet their needs.
If DME help them to maintain their independence in their home, they are considered as part of their needs.
Equipment not covered by Medicare, such as toilet safety frames, bathtub lifts, grab bars, if judged medically necessary, and within the person’s allotted budget, can be purchased on some of these programs or waivers.
To find out more about Medicaid Self Direction, click here.
Programs designed to transition people back from care institutions, into their own homes
Money Follows The Person
This is a Medicaid program which relocates the elderly back to their homes – which, as I said previously, can also mean assisted living – after they have been in nursing facilities.
If particular equipment is required so that the participant may relocate home, the program will purchase the equipment for them.
The range of equipment considered as DME is again much less restricted than under Medicare.
How to find the HCBS programs, waivers and 1915 waivers in your state
To find out what HCBS Waivers, 1915 Waivers, HCBS Programs and the Money Follows The Person Programs for seniors exist in your state, you can check my list of what is available in per state, along with links to the different program websites. I have also added PACE programs – Programs of All-inclusive Care for the Elderly in the home – “Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”.
What is the path to acquiring DME with Medicaid and state waivers, and HCBS programs ?
Step 1
– the doctor, or therapist, must provide a medical justification letter, which states that the equipment desired is medically necessary.
Step 2
– find a DME supplier, one who is Medicaid approved, and pass on to them the medical justification letter from the doctor, or therapist.
Step 3
– the DME supplier should then fill out a Prior Approval Application for Medicaid
Step 4
– the document goes to the Medicaid State Office for approval or denial
Step 5
– if unsuccessful, your loved one will be notified as to the reasons why, and told how to appeal the decision
Step 6
– if approved, you will receive the DME
If your income is a bit too high to qualify for Medicaid
Spend Down Programs
Medicaid Spend Down programs work to lower a program participant’s income level, or the income level + asset level, so that they may qualify for Medicaid coverage, by allowing the deduction of certain medical expenses, debt and loan payments.
The two methods of “Spending Down” –
- Income Spend Down
- Asset Spend Down
Income Spend Down is the simpler of the two methods, and allows a participant to deduct certain medical expenses from their income.
I’ve written a short post about how it works, which you can find here – What is Spend Down ?
How to find your State Medicaid State Agency
If all the technical jargon was too much for you, I would contact your state Medicaid Agency, and you can do that here.
Step 1 – Once you have clicked the link to Medicaid.gov, look at the section I have outlined in the image below
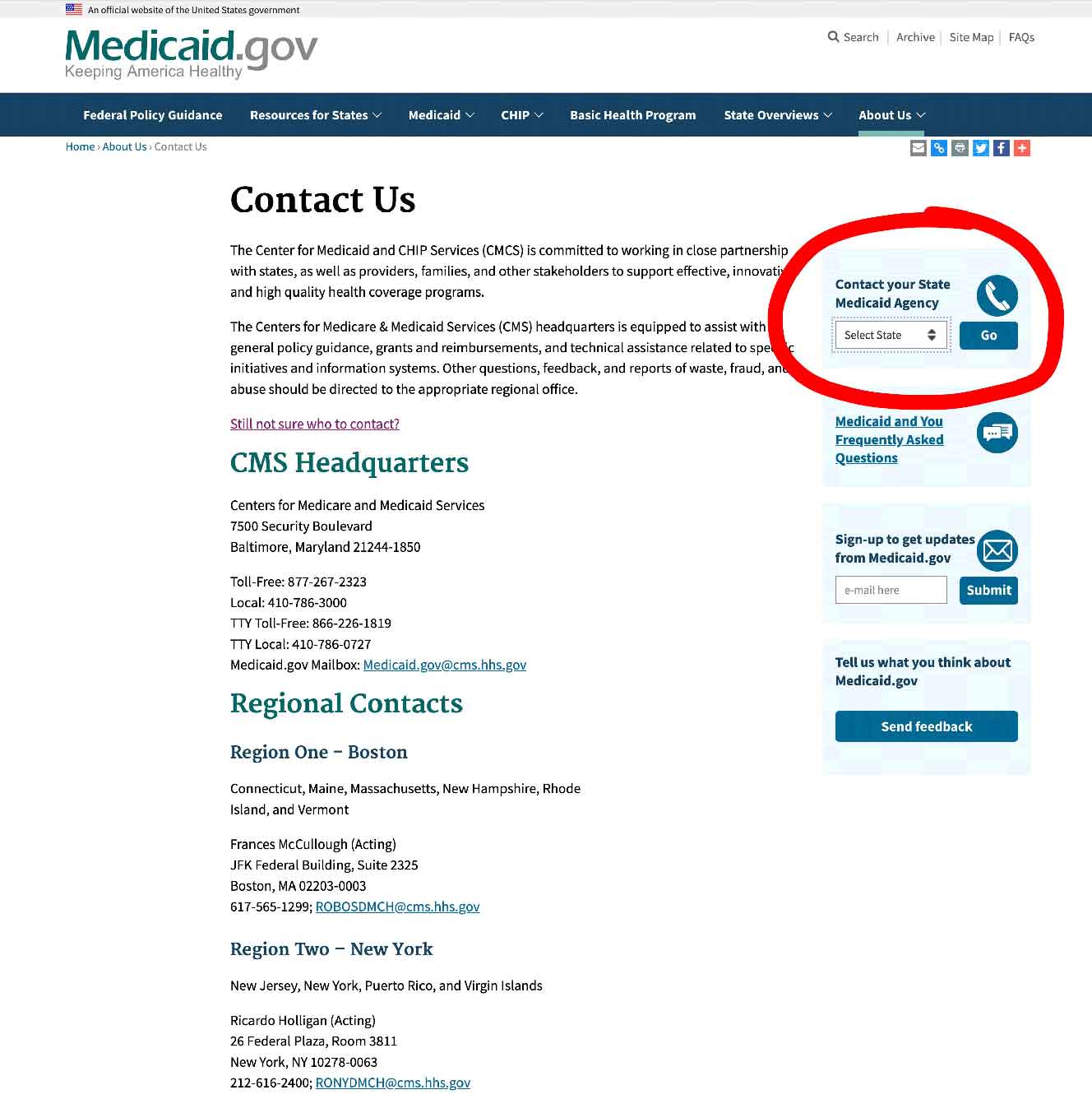
Step 2 – select your state, and click on “GO” – it will take you to your State medicaid Agency.
How to get a toilet safety frame covered as a Veteran ?
For veterans, the Department of Veterans’ Affairs has grants, programs, financial assistance and pensions which can help to cover the cost of DME.
To find out about your loved one’s local VA Medical Centers, Clinics and offices, click this link here.
Here are some of the forms of assistance available if your loved one is a veteran.
- Grants for remodeling homes due to disabilities inflicted during military service
- Veterans Direct HCBS – works like self direction
- Veteran Pensions – certain pensions allow for the purchase of medical equipment that veterans need for their homes, and the money is not lost to the pensioner
The range of DME is far wider than that available under Medicare.
State funding assistance
Assistive Technology Programs
Each state in the US receives a grant for an Assistive Technology Program.
These AT programs exist to increase access to assistive devices in the home.
The elderly are one of the primary groups who are meant to benefit from these programs.
The terms “Assistive Technology” and “DME” are basically interchangeable, and all manner of equipment which can help in the home is covered.
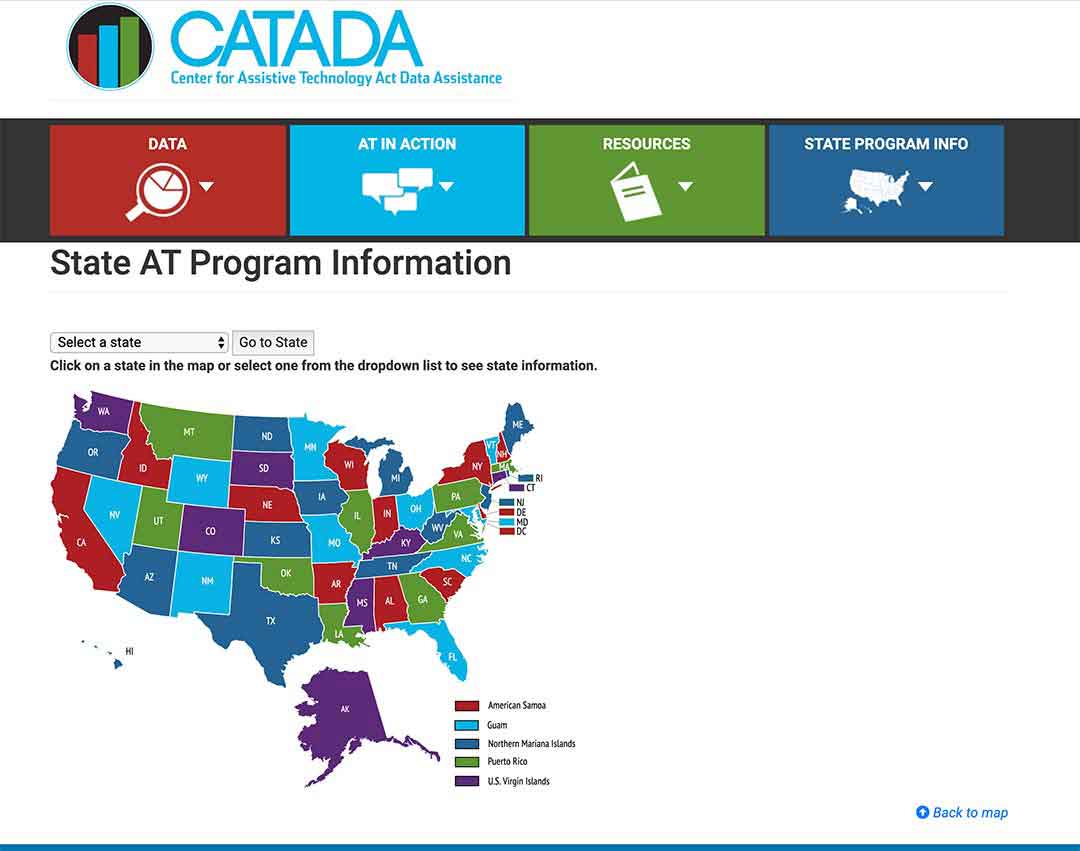
Check out what programs your state runs here.
Step 1/
Select your state on the map or from the drop-down menu and click on the button “Go to state”
– I chose Florida for this example
Step 2/
Look for the link “Program Title” – for my example I outlined it in red – and click on that.
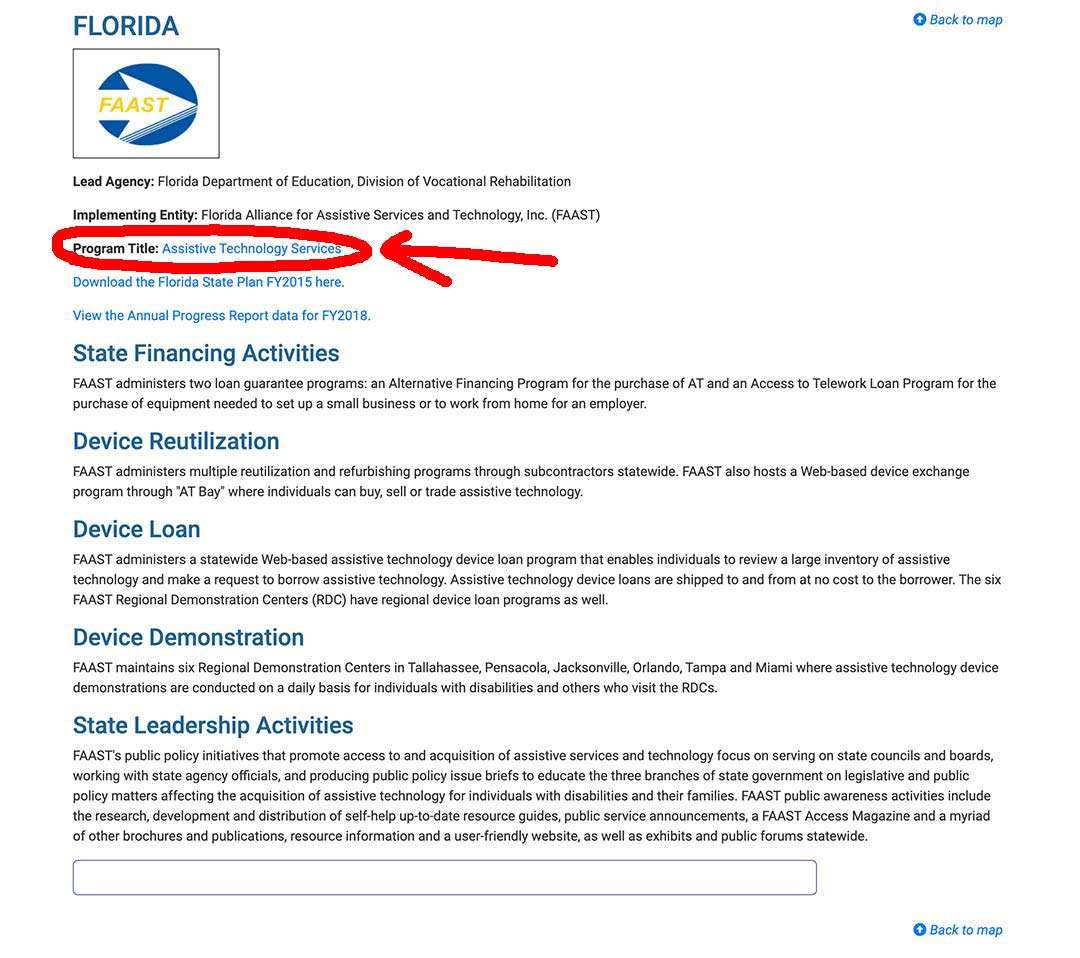
Step 3/
The State AT Program website will come up, and you can sign up, or use their contact info, to get in touch and find out what they offer to help the elderly, and if you, or a loved one, are eligible.
State Financial Assistance Programs
These are non-Medicaid programs to reduce the number of elderly persons entering into the Medicaid run nursing homes.
The programs are run on a state-by-state basis, and are designed to help the elderly to remain living independently in their own homes.
Not all the states have one.
The programs are destined for the elderly and disabled, but eligibility differs with each program.
The programs will modify homes and purchase any necessary medical and safety equipment.
USDA Rural development Section 504 Home Repair program
In rural areas, the elderly may obtain a grant for home remodeling and safety equipment –
“repair, improve or modernize their homes or grants to elderly very-low-income homeowners to remove health and safety hazards.” – source USDA.GOV.”
To qualify, you must –
- be the owner of the property
- be 62 yrs and over
- have a family income of less than 50% of the local average
- be unable to repay a home repair loan
Applications are accepted year round at your local Rural Development office here.
To talk to a local USDA Home loan specialist for advice, click here.
Protection and Advocacy Programs
Providing the elderly with legal assistance in disputing denied claims.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.