This week I have been taking a good look at different types of wrist braces, as I am trying to find something that could help my Mom with an arthritic, and rather weak wrist. And as usual, I am also looking at how much this will cost …
Does Medicare cover wrist braces ? Yes, Medicare Part B covers “medically necessary” wrist braces, as well as wrist supports and splints, if they have been prescribed by a Medicare-enrolled doctor, and acquired through a Medicare-approved supplier.
Contents Overview & Quicklinks
Medicare’s qualifying guidelines for a wrist brace
Medicare-approved wrist braces ?
Does Medicare cover back braces ?
Medicare’s qualifying guidelines for a back brace
Medicare-approved back braces ?
How much does Medicare pay for a back brace ?
Does Medicare cover knee braces ?
Medicare knee brace qualifying guidelines
Does Medicare cover “walking boots” ?
Does Medicare cover bathroom equipment ?
Medicare 5-year replacement rule
What equipment does Medicare cover ?
How do you get coverage from Original Medicare Part B for DME ?
Once you have a signed prescription, what’s next ?
Medicare-enrolled durable medical equipment supplier near me ?
What if you have a Medicare Advantage Plan ?
List of Durable Medical Equipment typically covered by Medicare
Free help with understanding Medicare
Does Medicaid cover wrist braces ?
Programs and waivers with the most flexible DME rules
How to find the HCBS programs, waivers and 1915 waivers in your state ?
How to get DME with Medicaid and state waivers and HCBS programs ?
Medicare qualifying guidelines for a wrist brace ?
Medicare Part B will typically cover 80% 0f the cost of a wrist and forearm brace if it is “medically necessary”, under the Benefit for Orthotics or Braces, and to qualify your wrist must need –
- stabilization of the wrist or forearm because of a weakness or deformity
- restriction of the movement of the wrist or forearm due to an injury or disease
- limitation of movement of the wrist or forearm during recovery from a surgical procedure on them
You will have to see a Medicare-enrolled doctor for a face-to-face appointment, and get a signed prescription certifying that you qualify, and the brace is “medically necessary”.
Medicare also covers splints and supports for wrist sprains and conditions such as carpal tunnel syndrome if your Medicare-enrolled doctor deems it “medically necessary” for you to have one.
Medicare-approved wrist braces
Medicare Part B gives coverage to both Custom Fitted and Off-the-Shelf wrist and forearm braces.
The difference between the two types of braces –
Custom Fitted braces –
Even though they may come as a kit, the custom fitted braces require fitting by a certified Orthotist, as they can require a significant amount of alteration during the fitting to make them fit correctly.
Off-The-Shelf braces –
These may be supplied as a kit that demands some assembly, but should require only a minimal adjustment by the beneficiary to fit properly, and do not require the help of a certified Orthotist for the best possible fit.
The passage below is from the Medicare Benefits Policy Manual Chapter 15 – Revised 2019 here.
130 – Leg, Arm, Back, and Neck Braces, Trusses, and Artificial Legs, Arms, and Eyes (Rev. 1, 10-01-03) B3-2133, A3-3110.5, HO-228.5, AB-01-06 dated 1/18/01
“These appliances are covered under Part B when furnished incident to physicians’ services or on a physician’s order.
A brace includes rigid and semi-rigid devices which are used for the purpose of supporting a weak or deformed body member or restricting or eliminating motion in a diseased or injured part of the body. Elastic stockings, garter belts, and similar devices do not come within the scope of the definition of a brace.
Adjustments, repairs and replacements are covered even when the item had been in use before the user enrolled in Part B of the program so long as the device continues to be medically required.”
Does Medicare cover back braces ?
Medicare Part B will cover back braces if they are “medically necessary” under the Benefit for Orthotics or Braces.
You will need to have a face-to-face appointment with a Medicare-enrolled doctor, and get a signed prescription certifying that a back brace is “medically necessary” in your case.
Medicare’s qualifying guidelines for a back brace
Medicare has guidelines about when coverage may be issued to a patient for a back brace, which the doctor has to check before giving you the signed prescription.
Medicare’s guidelines for back braces, which they are calling “Spinal Orthosis”
“A spinal orthosis (L0450 – L0651) is covered when it is ordered for one of the following indications:
1. To reduce pain by restricting mobility of the trunk; or
2. To facilitate healing following an injury to the spine or related soft tissues; or
3. To facilitate healing following a surgical procedure on the spine or related soft tissue; or
4. To otherwise support weak spinal muscles and/or a deformed spine.
If a spinal orthosis is provided and the coverage criteria are not met, the item will be denied as not medically necessary.”
In short, if you are to get coverage for the back brace, it must do one of the following for you –
- reduce pain by restricting movement of the torso
- promote with the healing of the spine or muscles, ligaments after an injury, or after surgery
- give support to a weak spinal muscle, and/or a deformed spine
If you do not qualify under one of these criteria, the doctor can’t prescribe the brace for you.
Medicare-approved back braces ?
Medicare will only cover rigid or semi-rigid braces of any type.
The two following exerts were taken from the Medicare Benefit Policy Manual, Chapter 15-
“A brace includes rigid and semi-rigid devices which are used for the purpose of supporting a weak or deformed body member or restricting or eliminating motion in a diseased or injured part of the body.”
The text goes on to say
“Back braces include, but are not limited to, special corsets, e.g., sacroiliac, sacrolumbar, dorsolumbar corsets, and belts.”
How much does Medicare pay for a back brace ?
Medicare Part B will pay 80 % of the Medicare-approved price for a back brace (semi-rigid or rigid), if it has been prescribed as “medically necessary” by a Medicare-enrolled physician and is purchased from a Medicare-approved DME supplier.
Do long as you have used a supplier who accepts assignment, you will pay your 20% co-inurance, and if you have not already done so, you will have to pay your annual deductible.
Does Medicare cover knee braces ?
Typically, a knee brace which has been prescribed by a Medicare-enrolled doctor as “medically necessary” will be covered by Medicare Part B.
You will need to have a face-to-face appointment with a doctor so that they can make the diagnosis, and then consider if your condition qualifies under the Medicare guidelines.
If you would like to read more about this, I have an article about Medicare and knee brace coverage. I cover the different types of brace, the conditions which qualify for coverage for a brace. If you aren’t eligible, I outline a number of different options including Medicaid and other state programs which can help if you qualify for those. You can read the article here.
Medicare knee brace qualifying guidelines
Of course, you must firstly be enrolled in Medicare Part B.
Medicare Part B requires that to get a knee brace, you have an in-person appointment with a Medicare-enrolled doctor so that they can make a diagnosis.
Medicare Part B covers knee braces as Durable Medical Equipment under the Orthotics or Braces Benefit if it is “medically necessary”.
Medicare says a knee brace is “medically necessary” when –
- a person is able to walk
- a knee requires stabilization because of weakness or deformity
- you have had a recent injury to the knee
- you recently had a knee surgery, such as a knee joint replacement
If you qualify, the doctor will give you a prescription certifying that your knee brace is “medically necessary”.
The doctor will doubtless tell you what type of brace you will need.
The text below, which is from Medicare, outlines the job braces must be able to do, and states that they can be either rigid, or semi-rigid.
Medicare Benefits Policy Manual Chapter 15 – Revised 2019 here
130 – Leg, Arm, Back, and Neck Braces, Trusses, and Artificial Legs, Arms, and Eyes (Rev. 1, 10-01-03) B3-2133, A3-3110.5, HO-228.5, AB-01-06 dated 1/18/01
These appliances are covered under Part B when furnished incident to physicians’ services or on a physician’s order.
A brace includes rigid and semi-rigid devices which are used for the purpose of supporting a weak or deformed body member or restricting or eliminating motion in a diseased or injured part of the body. Elastic stockings, garter belts, and similar devices do not come within the scope of the definition of a brace.
Adjustments, repairs and replacements are covered even when the item had been in use before the user enrolled in Part B of the program so long as the device continues to be medically required.
Medicare-approved knee braces
Medicare approves four types of knee braces
Medicare coverage includes four types of knee orthotics.
Devices must help manage stability or give pain relief and allow the patient to carry out daily functions.
Functional – A functional brace stabilizes the joint and control the movement to prevent any further traumas to the knee – for knees which have been injured and after knee surgeries.
Rehabilitative or Postoperative – these braces protect ligaments and tendons after surgery by limiting potentially harmful movements during the rehabilitation.
These braces may be used to prevent a recurring injury.
Unloader or Off-loader – these braces are built to take the stress off the knee.
The pressure is taken off the sides of the knee by restricting the sideways movement, and by putting the pressure on the thigh in order to take the stress off the joint.
They are often to reduce pain from osteoarthritis.
Prophylactic – these are also worn to prevent further injury to the knee and MCL ligaments by athletes at risk.
Custom Fitted and Off-The-Shelf
Medicare Part B allows both Custom Fitted and Off-the-Shelf knee braces.
Custom Fitted braces –
Custom fitted braces need to be by a certified Orthotist, as they may need significant amounts of alteration, to make them fit correctly.
Off-The-Shelf braces –
Off-The-Shelf braces do not require the help of a certified Orthotist for the best possible fit.
These may be supplied as a kit, but that should require only a minimal adjustment for you to fit them properly.
Does Medicare cover “walking boots” ?
Medicare Part B will typically cover 80% of the cost of a “walking boot”, or ankle/foot orthosis, as Durable Medical Equipment (DME) under the benefit for Orthotics or Braces.
Medicare will cover the “walking boot”, or ankle/foot orthosis –
- if the “walking boot” is either rigid or semi-rigid – not soft
- if the “walking boot” is being used to immobilize the foot/ankle after orthopedic surgery or for an orthopedic condition
Medicare does not give coverage if the boot is used to relieve pressure from foot ulcers, or other conditions, which may cause such sores on the feet.
Medicare covers foot ulcers under therapeutic shoes.
Does Medicare cover bathroom equipment ?
Some types of equipment you won’t be able to get coverage from Medicare Part B for, even though they may seem to be very important for the prevention of accidents for the elderly.
This is because safety devices are not generally medical in nature, and so can’t be classed as “medically necessary”.
Other items which Medicare Part B considers to be just “for comfort” or “for convenience” don’t qualify either.
So, unfortunately, you are going to find that almost all of what could be considered safety equipment for the bathroom is not covered by Medicare.
Equipment for bathroom safety not covered by Medicare Part B –
- grab bars
- raised toilet seats
- bath lifts
- bath seats
- floor to ceiling poles
- shower chairs
- bath chairs
- transfer seats
- toilet safety frames
Medicare Part B does cover the following equipment if it is prescribed as “medically necessary” for use in the home –
- crutches
- walkers
- bedside commodes
Luckily, if you can get coverage for these items, they can be used in the bathroom to help with stability and mobility issues.
If you have a Medicare Advantage Plan (these are private companies offering Medicare) you may have a little more luck, as the number of benefits allowed was expanded in the fall of 2020, and the types of benefits can include certain equipment for individuals with chronic illnesses, which includes some bathroom safety equipment.
This is a very recent development it may yet be rather hard to find too many plans offering much in the way of bathroom safety equipment where you live, but it is coming, and it is only on Medicare Advantage Plans, not Original Medicare.
Medicare 5 year replacement rule
Medicare Part B replaces covered DME that are –
- worn out through use
- that have always been in your possession
- too worn out to be fixed
- the minimum period considered to be a lifetime for DME is five years
- the lifetime can vary depending on the type of equipment (knee braces last 1-2 years)
Medicare will cover the repair of worn out items which haven’t reached the end of their lifetime, but not more than the cost of a replacement item.
When replacing an item, the claimant has to go through the whole procedure of having an appointment with a Medicare-enrolled doctor to get a new prescription for the replacement item.
What equipment does Medicare cover ?
Equipment that Medicare covers for use in the home is called “durable medical equipment”, or DME.
For equipment to qualify as durable medical equipment, it must –
- be able to withstand constant use over time – durable
- be primarily medical – not for comfort
- be only of use to a sick person
- be primarily for use in the home
- have a lifetime of at least 3 years
How do you get coverage for a wrist, knee or back brace from Medicare Part B for DME ?
To be able to be covered by Original Medicare Part B for durable medical equipment for “use in the home” –
- you must be enrolled in Medicare Part B
- you have to have a Medicare-enrolled doctor to give you a signed prescription which certifies that the DME is a “medically necessary”
- your equipment supplier must be a Medicare-enrolled supplier
For Medicare’s purposes, “living at home” means –
- living in your own home
- living in the family home
- living in the community, such as assisted living
Once you have a signed prescription, what’s next ?
Now you can get your DME –
- it’s time to visit a Medicare-enrolled DME supplier
- be sure the supplier is a Medicare-enrolled “participating” supplier who accepts “assignment’ – this guarantees you pay only 20% of the Medicare-approved price
- despite the fact that Medicare only covers the most basic of models, you can sometimes, if you pay extra, get upgrades
- select your DME that you have been prescribed from those on offer
- sort out the necessary paperwork in compliance with Medicare’s rules
So, long as you used a Medicare-enrolled supplier and the prescription is from a Medicare-enrolled doctor certifying that the DME is “medically necessary”, Medicare part B will typically cover 80% of the Medicare-approved price for DME.
If you have used a Medicare-enrolled “participating” supplier who accepts “assignment”, you will only have your Medicare coinsurance payment of 20% of the Medicare-approved price to pay for the DME, plus your annual deductible if it applies.
Always use a Medicare-enrolled supplier who is a Medicare-enrolled “Participating” supplier who accepts “assignment”, If you don’t, you pay so much more than you need to.
Medicare will either rent or purchase your DME – when Medicare rents the DME, rather than buying it, the payment structure remains the same – you will still pay a 20% coinsurance payment, but of the monthly rental fee, and you will pay it each month.
Medicare-approved durable medical equipment supplier near me
You can use this link to find a Medicare-enrolled supplier who is local to you – Medicare.gov>
What if you have a Medicare Advantage Plan ?
Medicare Advantage plans are Medicare offered by private companies under contract with Medicare, and they cover, at a minimum, at least everything covered by Original Medicare and sometimes, depending on the plan, some extras.
So, as wrist braces are covered by Original Medicare, so they are also covered by Medicare Advantage plans.
You will need to contact your plan provider, to get all the specifics about doctors and suppliers, as they will use their own network, and won’t provide coverage if you go outside it.
List of durable medical equipment covered by Medicare
If you don’t find the equipment you are looking for in my list of Medicare covered DME below, you can use this link to Medicare.gov
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
Free help with understanding Medicare
SHIP – State Health Insurance Assistance Programs
Free counseling services for Medicare, Medicaid and Medigap are available from your state program.
Here’s a short guide outlining how to find your local SHIP – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Does Medicaid cover wrist braces ?
Medicaid programs in each state are funded both federally, and by the individual state itself.
Consequently, each individual state, so long as it follows the Medicaid guidelines, has quite a lot of leeway in what it does on its Medicaid programs.
Medicaid will often let a state waive particular eligibility requirements for some of their programs, so that the state may be able to give health care to a certain demographic, which might otherwise be neglected.
When this occurs, it’s known as a waiver.
A waiver can have its own specific eligibility requirements, and typically a limited number of places for participants.
There are literally hundreds of waivers, all with different eligibility criteria, across the US.
Care in the home – Medicaid and state programs
“Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers”
These are programs which have been established for low income families, the disabled and the elderly.
The programs provide the participants with health care services in the home, so as they may be able to remain in their homes living independently.
To help the elderly participants to maintain their independence, these programs and waivers, will all help purchase “home medical equipment”, and very often they pay for it all.
You can find out if you are eligible for an HCBS program, or waiver, by contacting your State Medicaid Agency here.
If you prefer, you can just visit your local Area Agency on Aging.
The link below will take you to more information about HCBS programs or waivers –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
Medicaid uses the term “home” to mean any of the following –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
Programs and waivers with the most flexible DME rules
HCBS programs and waivers using “Consumer Direction” or “Self Direction” systems of budget self-management
This is a type of program structure where the participant self-manages their allocated budget across their needs, albeit with the assistance of an appointed financial advisor.
The participants choose the medical and safety equipment which is necessary to them being able to maintain their independence, and if it is covered by their budget, they are allowed to purchase it.
There is greater scope for what can be considered DME on these programs than on Medicare.
Learn more about Medicaid Self Direction here.
Money Follows the Person
The program Money Follows The Person is a federal Medicaid program, which was established to assist elderly adults living in nursing homes to move back to their own homes.
The Medicaid program helps the states with the necessary funding to set up their own Money Follows The Person programs.
The states will either use HCBS waivers which already exist to assist the elderly in making the transition back to their homes, or they will use the funding to design, and establish, new programs for those purposes.
These programs will give money for all sorts of equipment, and also for any remodeling which is required for the move.
How to find the HCBS programs, waivers and 1915 waivers in your state
To find the Medicaid HCBS waivers and programs for seniors in your state, you can take a look at my guide listing them by state, as well as the Money Follows The Person Programs and PACE Programs (Programs of All-inclusive Care for the Elderly). The guide is here – “Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”.
How to get DME with Medicaid and state waivers and HCBS programs ?
Step 1
– the doctor, or therapist, has to provide a medical justification letter, stating it is medically necessary
Step 2
– find a Medicaid-approved DME supplier, and give them the medical justification letter
Step 3
– the Medicaid-approved supplier fills out a Prior Approval Application form for Medicaid
Step 4
– the Prior Approval Application is sent to the Medicaid State Office
Step 5
– if you are unsuccessful you will be contacted and given the reasons as to why, as well as advice on how to make an appeal
Step 6
– if approved, you will receive the DME
If your income is a bit too high to qualify for Medicaid
Spend Down Programs
In short, Medicaid Spend Down programs work to reduce a program participant’s income level, or the income level + asset level, so that they may qualify for Medicaid coverage, by allowing the deduction of certain expenses.
The two methods are called –
- Income Spend Down
- Asset Spend Down
Income Spend Down is the simpler of the two methods, and basically allows a participant to deduct certain medical expenses from their income.
I’ve written a short post about how it works, which you can find here – What is Spend Down ?
To find your State Medicaid State Agency
If you just want to talk to, or to email someone, contact your state Medicaid Agency here.
Step 1 –
Click the link to Medicaid.gov, look to the section I outlined in red.
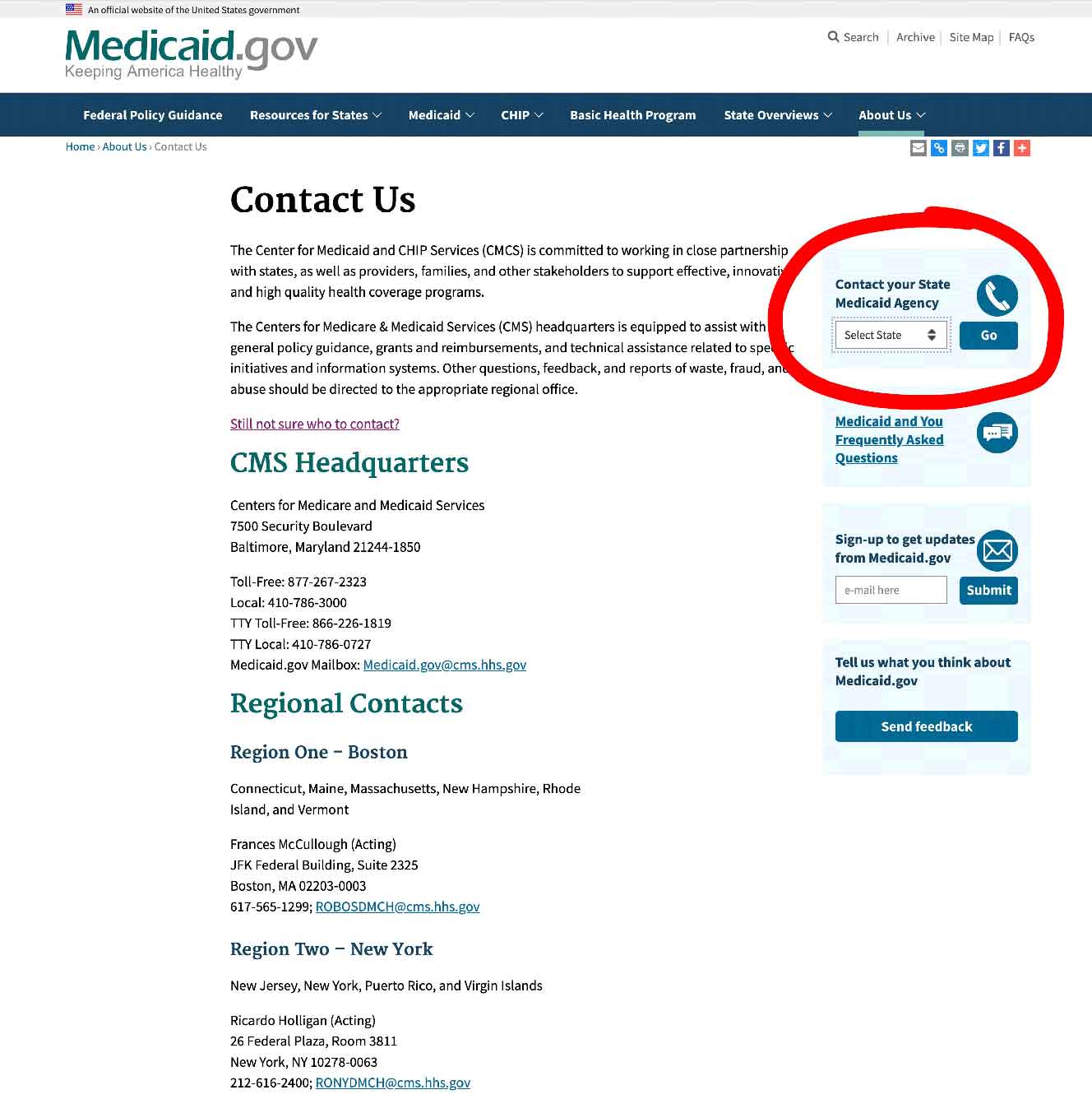
Step 2 –
Select your state and click on the button they have marked “GO” – it will take you to your State Medicaid Agency with all their contact info.
State Funding Assistance
Assistive Technology Programs
Assistive Technology Programs are present in each state, and are another example of a program whose primary focus is on the elderly and the disabled.
The goal of the programs is to improve access to assistive devices in the home,
The classification “Assistive Technology” is somewhat similar to “Durable Medical Equipment”, but as well as medical items it also covers equipment which facilitates users to accomplish activities they otherwise could not. This could be anything from dressing for the arthritic through to digital tablets and communication devices.
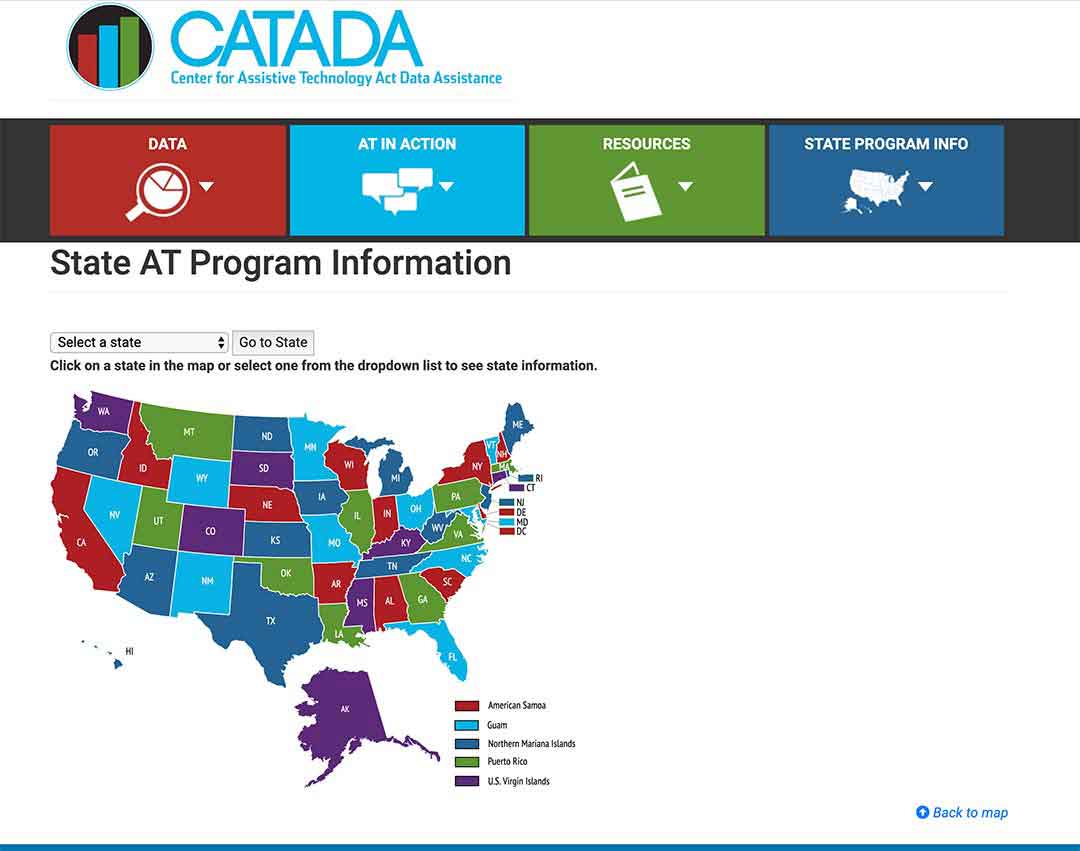
To find out what projects your state runs, click here.
Step 1/
Pick your state on the map or the drop-down menu, and click on “Go to state”
– I chose Florida for this example
Step 2/
Click on the link “Program Title” – for my example, I outlined it in red.
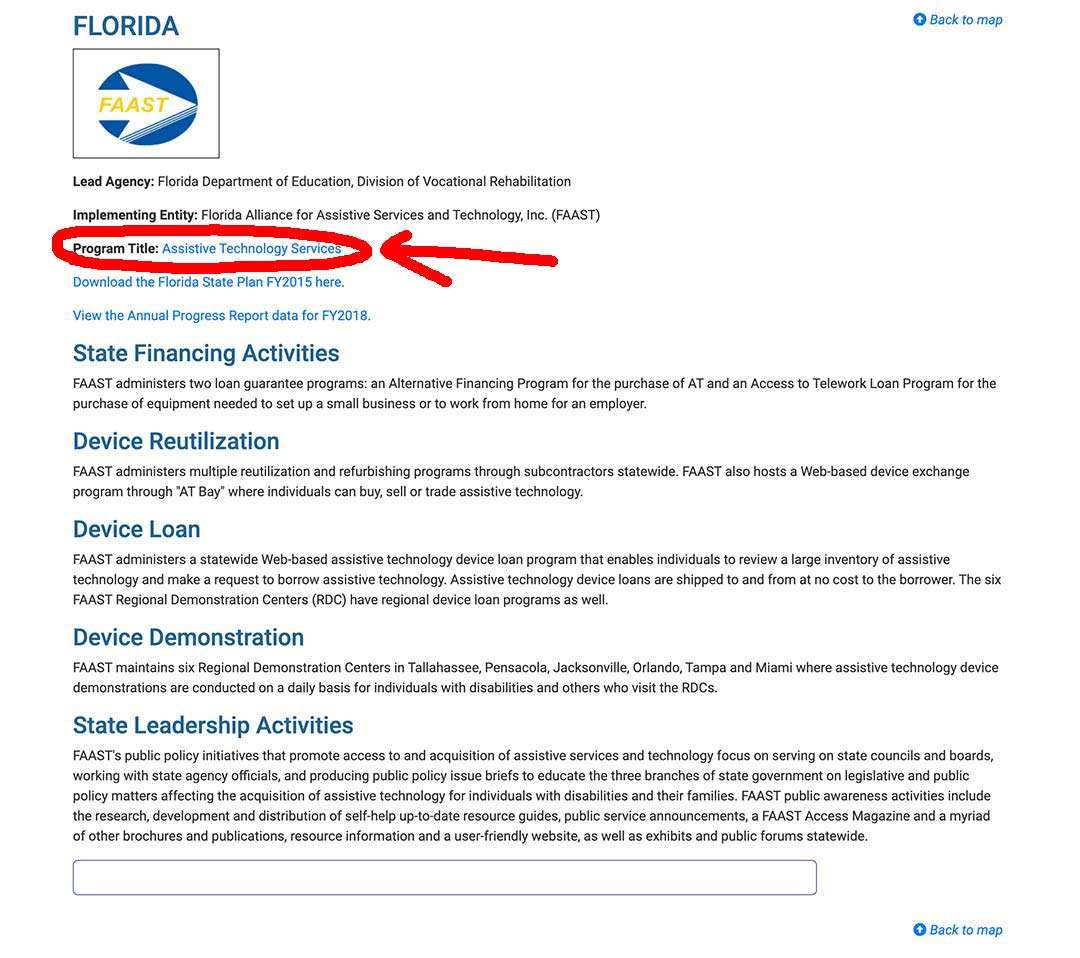
Step 3/
The AT Program state website will come up, and you can sign up, or use their contact info .
State Financial Assistance Programs
You can find non-Medicaid programs in some states which focus on helping the participants to remain living in their homes.
In order to achieve their goals, the programs will give the participants grants, or loans, or a combination of the two.
The money can be used to pay for safety equipment, assistive equipment, the remodeling of bathrooms and kitchens, wheelchair ramps – the participants’ medical and safety requirements for living securely in their homes are covered to a great extent by the programs.
The main target groups for such programs are the elderly and the disabled.
The best place to find out if your state has one of these programs is your local Area Agency on Aging.
Summary
Wrist braces, rigid and semi-rigid, qualify as Durable Medical Equipment for Medicare.
With Medicare part B, under certain conditions, you can get coverage for rigid and semi-rigid wrist braces, so long as you have a signed prescription from a Medicare-enrolled doctor certifying that its “medically necessary”.
You should always acquire your brace from a Medicare-enrolled “Participating” supplier who accepts “assignment” so that you will only have the co-payment of 20% of the Medicare-approved price, and your deductible if it applies.
Medicare also covers back, elbow, ankle/foot and knee braces under certain conditions.
Medicare Advantage covers the same braces as it has to offer the same coverage as Medicare. It will also, depending on the plan provider, have its own extras, but you will have to check what those may be with your plan provider, if you have an Advantage plan.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.

