One of the largest, and most costly items, that seniors may need to consider purchasing to maintain independence in their home is an adjustable bed, so finding out how to pay for one is important.
Medicare Part B will typically cover adjustable beds as durable medical equipment for use in the home, if the bed is prescribed as “medically necessary” by a physician.
Contents Overview & Quicklinks
Which adjustable beds does Medicare cover ?
What types of hospital bed will Medicare Part B pay for ?
Medicare requirements for a hospital bed
Medicare qualifying diagnosis for a hospital bed ?
Does Medicare Advantage cover hospital beds ?
What are the payment options for an adjustable bed with Medicare Part B ?
How much does a hospital bed cost ?
How much does it cost to rent a hospital bed ?
Where can I rent a hospital bed locally ?
How often can you get an adjustable bed with Medicare ?
What is the procedure for getting an adjustable/hospital bed at home with Medicare coverage ?
What do you do once you have the 0rder/prescription ?
Why you should always use a Medicare-enrolled “participating” supplier
Why is it less expensive with a Medicare-enrolled “participating” supplier ?
If you don’t use a “Participating” Supplier, what’s the result ?
What if you are being treated in a nursing facility ?
Durable medical equipment, which is typically covered by Medicare
Durable medical equipment, which is typically not covered by Medicare
Free assistance with understanding Medicare
Does Medicaid pay for an adjustable ?
How to find the HCBS programs, waivers and 1915 waivers in your state ?
How do you acquire DME with Medicaid and state waivers and HCBS programs ?
What if your revenue is a too high to qualify for Medicaid ?
Other state assistance for finding hospital beds for the elderly
What is an adjustable bed ?
An adjustable bed is a which has separate parts of the bed which can be raised, or lowered, independently of one another, such as the head or foot sections of the bed.
The beds can be very basic and fully manual, or can be fully electric, with lots of extra functions including massage and heat options.
Which adjustable beds does Medicare cover ?
Medicare typically covers certain basic hospital beds as durable medical equipment for use in the home, under certain conditions. The beds are the very basic models.
If necessary, your physician can order certain extras – certain mattress pads, bed rails and an air-fluidized bed.
DME adjustable beds
The medical equipment which is covered by Medicare Part B, for use in the home, is called “durable medical equipment”, or DME.
The basic hospital beds, which I noted above, qualify as durable medical equipment.
For Medicare, durable medical equipment must fit the following criteria :-
- Durable (can withstand repeated use)
- Used for a medical reason
- Not usually useful to someone who isn’t sick or injured
- Used in your home
- Generally has an expected lifetime of at least 3 years
Source: Medicare.gov website – here
Original Medicare Part B covers durable medical equipment which is prescribed as “medically necessary”.
Original Medicare Part B doesn’t cover what Medicare considers to be comfort items, such as raised toilet seats, air purifiers or a wedge pillow.
What types of hospital bed which Medicare Part B will pay for
Original Medicare will not provide cover for just any adjustable bed for use in the home, but it will cover for a basic hospital bed which is not fully electric.
You can, though, pay the difference out of your own pocket to get a fully electronic bed.
Hospital beds are a type of adjustable bed, but are designed to be easily maintained and cleaned.
The hospital beds will have height, and angle, adjustable areas under –
- the head and shoulders at the top of the bed
- the feet and lower leg
The height of the whole bed may also be adjustable.
Medicare negotiates with suppliers to obtain a certain price for certain beds, and those are the models which are going to be covered by Medicare.
For this reason, it’s important to stick to the correct procedure if you want to be covered.
Here are the types of bed covered by Medicare –
Manual hospital bed
These beds are fully manual, and are adjusted by turning a crank.
The number of cranks may vary.
Of all the hospital beds, these are the most economical, but also the most physically demanding for the carer.
Variable height hospital bed
Variable height beds are a type of manual bed, with the added option of adjustable height.
The bed has the options to adjust the head and foot sections of the bed, and the option of changing the overall bed height.
The adjustments are made using a hand crank.
Semi-electric hospital bed
With semi-electric beds, motors are used to adjust the head and foot sections of the bed, and a manual crank is used to adjust the height of the bed.
The electric motors are controlled with a hand held device, allowing the bed occupant the to adjust the head, and foot, sections for themselves without need of assistance.
Although, the user will still need to have a carer to adjust the overall height of the bed with the crank.
Bariatric or “Heavy Duty” Hospital bed
Bariatric or heavy-duty hospital beds are made for heavier individuals.
The two weight categories for bariatric hospital beds which Medicare covers are –
- 300 lb to 600 lb – Heavy Duty extra wide hospital beds
- 600 lb and above – Extra Heavy Duty hospital beds
Medicare requirements for a hospital bed
To qualify for Medicare Part B coverage for a hospital bed as durable medical equipment for use in your home, you must –
- be enrolled in Medicare Part B (this is the part which covers outpatient costs, i.e. in the home in this case)
- have a signed prescription from a physician certifying that the bed is “medically necessary” according to the Medicare criteria
- the physician who prescribes the bed must be a Medicare-enrolled physician
- have had an in-person visit with the physician within 6 months prior to the ordering of the bed
- have a qualifying diagnosis
- your physician must present case history documents
- your physician has to show how you will benefit from having a hospital bed – either maintaining it or improving it
- use a Medicare-enrolled durable medical equipment supplier, preferably a “participating” supplier
Medicare qualifying diagnosis for a hospital bed ?
Original Medicare Part B will partially cover a hospital bed for use in the home if you meet one or more of the following criteria:
- If you have a medical condition “which requires positioning of the body in ways not feasible with an ordinary bed. Elevation of the head/upper body less than 30 degrees does not usually require the use of a hospital bed, or”
- You require “positioning of the body in ways not feasible with an ordinary bed in order to alleviate pain, or”
- You require “the head of the bed to be elevated more than 30 degrees most of the time due to congestive heart failure, chronic pulmonary disease, or problems with aspiration. Pillows or wedges must have been considered and ruled out, or”
- You require “traction equipment which can only be attached to a hospital bed.”
Variable Height Hospital Beds – beds that allow the height of the bed to vary can be covered if you have met one or more of the principal criteria above, and require “a bed height different than a fixed height hospital bed to permit transfer to chair, wheelchair or standing position.”
Semi-electric Hospital Beds – can be covered if you have met one or more of the principal criteria above, and require “frequent changes in body position and/or has an immediate need for a change in body position.”
Heavy Duty Extra Wide Hospital Beds – can be covered if you have met one or more of the principal criteria above, and your “weight is more than 350 pounds but does not exceed 600 pounds.”
Extra Heavy Duty Hospital Beds – can be covered if you have met one or more of the principal criteria above, and your “weight is more than 600 pounds”
Total Electric Beds are not covered as they are deemed by Medicare to be a convenience feature, and they are “denied as not reasonable and necessary.”
The guidelines are from the CMS (Centers for Medicare and Medicaid Services) Requirements list for Hospital Beds and Accessories.
There is a much more technical document which you can read on CMS.gov – National Coverage Determination (NCD) for Hospital Beds (280.7) – here.
Does Medicare Advantage cover hospital beds ?
If you have a Medicare Advantage Plan (often called Medicare Part C) you should be able to get a bed covered by the plan if it is considered “medically necessary” by Medicare, but you must consult with your plan provider.
Medicare Advantage Plans are run by private companies, which are contracted by Medicare to provide Medicare services, and are bound by law to provide, at least, the same coverage as Original Medicare Parts A and B.
The companies providing these plans will have their own requirements for a claim.
Almost certainly, you will have to use a DME supplier in their network, otherwise you really are risking having to pay the whole bill for the bed yourself.
What are the payment options for an adjustable bed with Medicare Part B ?
The payment method for the bed will depend on the model type and the supplier you use, but it will be either –
- a rental
- a purchase
So long as your doctor is a Medicare-enrolled doctor, and the supplier also is a Medicare-enrolled supplier, then Medicare should accept to cover the purchase and –
- your deductible for Medicare part B will apply
- you will need to pay the supplier your co-pay of 20% of the Medicare-approved price of the item
- Medicare will then pay the supplier the remaining 80% of the Medicare-approved price for your item
How much does a hospital bed cost ?
Hospital beds range in price from $500.00 to $12,000.00 – not including highly specialized ICU beds.
Let’s now take a look at the cost of the types of bed for which Medicare offers 80% coverage for if you are enrolled and qualify under their criteria – Medicare will typically only cover the most basic hospital beds.
The following prices are taken from normal medical supply retailers, so will most likely be higher than those paid by Medicare – Medicare makes contracts with their approved suppliers, giving them lower prices.
The prices are for standard sized single hospital beds, they do not include the mattress or side rails –
Manual hospital beds – no electric parts – $500.00 – $800.00
Variable height manual hospital bed – $550.00 – $700.00
Semi electric hospital beds – $550.00 – $900.00
For larger individuals, Medicare covers Heavy Duty and Extra Heavy Duty hospital beds –
Heavy Duty hospital bed (300lb – 600lb) – $1750.00 – $4000.00
Extra Heavy Duty Hospital bed (600lb and above) – $3875.00 – $7,000.00
How much does it cost to rent a hospital bed ?
Depending on a person’s situation, and the length of time the bed will be required, Medicare may give the choice of either purchasing the bed, or renting it.
When a hospital bed is rented with Medicare coverage, it is what is called a “capped rental” item, renting the hospital bed for 13 monthly payments, at the end of which the beneficiary will own the bed.
Medicare will only cover certain types of hospital bed, and typically only up to 80 % of the Medicare-approved cost, if they are prescribed by a Medicare-enrolled physician and if they are bought from a Medicare-enrolled supplier.
The typical cost of renting a hospital bed is $200 – $500 a month to rent.
If you’re renting with the typical Medicare Part B coverage of 80%, you will then pay 20% of the rental cost.
Example – if the bed rental was $250 per month, Medicare Part B would pay the medical supplier $200 towards the rental each month, and you would pay your coinsurance of $50 each month.
If your deductible applies, you would have to pay that as well at the outset.
For larger items, the cost is more easily managed by paying a monthly rental.
Medicare adjustable bed suppliers
If you want to find a Medicare-enrolled Durable Medical Equipment supplier near you, use this link to the Medicare.gov locator tool.
You can also check Medicare’s documentation on Durable Medical Equipment here – Mediace.gov
If your doctor is participating in Medicare, they should have all of this information and order the bed for you.
How often can you get an adjustable bed with Medicare ?
If you have had a DME in your possession for its whole lifetime, which is worn out, Medicare will replace it.
For equipment replacement, the lifetime of a DME cannot be less than 5 years. The equipment must be worn out from use to replace it.
Medicare only replaces like for like – you can’t get an item upgraded.
What happens if a DME is damaged or stolen?
If any DME covered by Medicare is lost, stolen, or damaged in an accident or a natural disaster, so badly that it can’t be repaired, Medicare will, as long as you have proof, replace it.
What’s the procedure for getting an adjustable/hospital bed at home with Medicare coverage ?
To Recap –
To get coverage for an adjustable bed for home use covered through Medicare Part B you will need to –
- be enrolled in Medicare Part B
- have a prescription/order signed by your Medicare-enrolled doctor, or treating practitioner, which states that it’s a medical necessity to have the bed
- be buying the bed from a Medicare-enrolled enrolled supplier
Should the Doctor, treating practitioner, or DME suppliers not be Medicare-enrolled, Medicare will not cover the purchase at all.
If you are claiming a hospital bed for your “home”, a hospital or nursing home does not qualify for coverage under Medicare Part B – skilled nursing facilities qualify under Medicare Part A (hospital insurance).
For someone living in a long-term care facility, such as an assisted living, it can qualify as “home” for under Medicare Part B.
The following can be considered living at “home” according to Medicare –
- you can be in your own home
- you can be living in the family home
- you can be living in the community, such as assisted living
What do you do once you have the order/prescription ?
Your doctor will order the hospital bed from a supplier with you.
In the case of cheaper items, Medicare will usually purchase the items.
With a hospital bed Medicare will most likely want to rent the bed on a monthly basis, the rental price being a Medicare-approved price, and you will pay the supplier your 20% co-pay of the monthly rental, plus you will have to pay your Medicare Part B annual deductible if it applies.
Why you should always use a Medicare-enrolled “participating” supplier
If you use a supplier who is not a Medicare-enrolled “participating” supplier, you may pay more than if you had used a Medicare-enrolled “participating” supplier.
Why is it less expensive with a Medicare-enrolled “participating” supplier ?
Firstly, to get any kind of cover from Medicare, you have to use a Medicare-enrolled supplier.
A Medicare-enrolled supplier has passed all of Medicare’s required standards of service and has agreed to take payment from Medicare.
But more importantly than that …
Medicare-enrolled suppliers are divided into two types –
- Medicare Suppliers
- Medicare “Participating” Suppliers
And Medicare “Participating” Suppliers have agreed with Medicare to accept what is known as “assignment” – most importantly, a supplier who accepts “assignment” can only charge the Medicare-approved price for DME.
As a result –
- the “participating” supplier will provide the documentation for your equipment for Medicare
- if your equipment claim is approved by Medicare, the “participating” supplier can then only ask for the 20% co-pay of the Medicare-approved price
- if your annual Medicare deductible applies, you will have to pay this as well
If you don’t use a “Participating” Supplier, what’s the result ?
A Medicare-enrolled supplier who is not a “Participating” Supplier –
- has agreed with Medicare to accept from them the payment for DME at the Medicare-approved price
- but can sell the DME to you, the buyer, at up to 15% more than the Medicare approved price
What this means –
- as agreed when your claim for a DME is submitted, if it is approved, Medicare will pay the supplier their 80% of the Medicare-approved price for your DME
- and you end up paying your 20% co-pay of the Medicare-approved price for your item + the difference between the Medicare-approved price and the price the supplier is selling the item at to you (with a limit of 15% extra)
- And you will have to pay your annual Medicare deductible if it applies
Some states, such as New York, restrict the supplier from charging a full 15% above the Medicare-approved price. In New York, they may only add 5%.
So do use a Medicare-enrolled “Participating” Supplier, and always ask if the supplier accepts “assignment”, as you can save a lot of money, particularly with an item as costly as a hospital bed. Don’t get burned !
What if you are being treated in a skilled nursing facility ?
If you’re being treated in a Skilled Nursing Facility or hospital, you will be covered by Medicare Part A (Hospital Insurance). The nursing facility under Medicare is required to provide any DME needed for 100 days.
Durable medical equipment, which is typically covered by Medicare
To qualify, you will need to have Original Medicare Parts A and B.
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
Corrective Lenses
Prosthetic Lenses
Cataract glasses (for Aphakia or absence of the lens of the eye)
Conventional glasses or contact lenses after surgery with insertion of an intraocular lens
Intraocular lenses
Important: Only standard frames are covered. Medicare will only pay for contact lenses or eyeglasses provided by a supplier enrolled in Medicare, no matter who submits the claim (you or your supplier).
Durable medical equipment, typically not covered by Medicare
Adult Diapers
Air Cleaners
Air Conditioners
Alcohol Swabs
Augmentative Communication Device
Bathroom Aids
Bathtub Lifts
Bathtub Seats
Bed Bath
Bed Boards
Bed Exit Alarms
Bed Sensor Pads
Bed Lifter
Beds – Lounge
Bed Wedges
Blood Glucose Analyzers
Braille Teaching Texts
Caregiver Paging Systems
Catheters – except those which are used for permanent medical conditions where the catheter is considered as a prosthetic
Chair Exit Alarms
Chair Sensor Pads
Communicator
Contact Lenses – Medicare helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens
Dehumidifiers
Dentures
Diathermy Machines
Disposable Bed Protectors
Disposable Sheets
Door Exit Alarms
Easygrip Scissors
Elastic Stockings
Electrical Wound Stimulation
Electrostatic Machines
Elevators
Emesis Basins
Esophageal Dilators
Exercise Machines
Exit Alarm Mat
Eyeglasses – Medicare helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens.
Fall Alarms
Fans
Fabric Supports
Fomentation Device
Grab Bars
Grabbers
Gauze
Hearing Aids
Heat and Massage Foam Cushion Pad
Heating and Cooling Plants
Home Modifications
Humidifiers – not room humidifiers
Incontinence Pads
Injectors (hypodermic jet pressure powered devices for Insulin injection)
Irrigating Kits
Insulin Pens
Massage Equipment
Motion Sensors
Motion Sensor Exit Systems with Pagers
Needles
Oscillating Beds
Over bed Tables
Paraffin Bath Units (if not Portable)
Parallel Bars
Portable Room Heaters
Portable Whirlpool Pumps
Preset Portable Oxygen Units
Pressure Leotards
Pressure Stockings
Pulse Tachometer
Pull String Alarms
Raised Toilet Seats
Ramps
Reading Machines
Reflectance Colorimeters
Sauna Baths
Special TV Close Caption
Speech Teaching Machines
Stair Lifts
Standing Table
Support Hose
Surgical Face Masks
Surgical Leggings
Syringes
Telephone Alert Systems
Television Assistive Listening Devices
Telephone Arms
Toilet Seats
Treadmill Exercisers
Walk in Bathtubs
Wheelchair Lifts
Whirlpool Pumps
White Canes
Wigs
If you are trying to qualify for an adjustable bed through Medicare because you wanted a bed with side rails, you may be interested to know that they are not the safest option for certain categories of elderly, or frail individuals, and have been linked to many deaths.
In the article “Alternative to bed rails for the elderly” I outline lots of safer options to stop your parents from falling out of bed, and which are also far less costly than a hospital bed. It is worth a look, and you can find that here.
Free assistance with understanding Medicare
SHIP – State Health Insurance Assistance Programs –
Your SHIP offers free counseling services on Medicare, Medicaid and Medigap for your state residents.
I have a short article explaining how to contact your local SHIP, and you can find that here –
“Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Will Medicaid pay for an adjustable bed ?
Medicaid doesn’t operate in the same way as Medicare, as it is joint federal and state funded. Each state runs its Medicaid program as it wishes, within the guidelines set out by the government, and this leads to there being differences from state to state as to what can be covered by Medicaid.
A state will have a Medicaid State Plan, and usually Home Community Based Services (HCBS), or waivers (also Medicaid), each with their own eligibility, criteria and goals, and resulting in hundreds of programs and waivers for Medicaid across the US.
With these hundreds of HCBS waivers and state plans, what can be considered durable medical equipment can vary from program to program, let alone from state to state.
Medicaid and state programs for in the home
Medicaid for home care, is called “Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers”.
The HCBS programs, or waivers, operate to help the recipients to maintain their independence in their own home, by providing the care and services required to these ends, and by paying for “home medical equipment”.
If you would like to find more technical, and in depth information, about the different waivers which exist, take a look at the official Medicaid site –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
The term “HOME” for HCBS programs and waivers, is used to mean that the beneficiary of a program, or waiver, must be living in –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
Medicaid waivers, which offer a greater chance of getting free DME
Some HCBS programs, or waivers, allow for what is called Consumer Direction/ Self Direction.
The program participant is allotted funding, or a budget, for their living needs in their home, which they spend with the help of a financial planner. Durable medical equipment can be purchased with this budget if it is part of what they need.
Equipment such as a bathtub, grab bars, a bath lift, or a shower chair, which isn’t considered durable medical equipment by Medicare, if it is considered “medically necessary” and is within the allotted budget, may be purchased by participants on some of these programs, or waivers.
To find out more about Medicaid Self Direction, click here.
There are also programs which are specifically developed to help with transitioning people from institutions back into their own homes –
Money follows the person is one such Medicaid program for helping people to leave nursing facilities, and to relocate them back to their own homes – this can include assisted living.
Any durable medical equipment which is considered to be necessary for the beneficiaries to return to, and to live in, their homes is bought by the program.
Once again, what qualifies as DME is less limited than for Medicare.
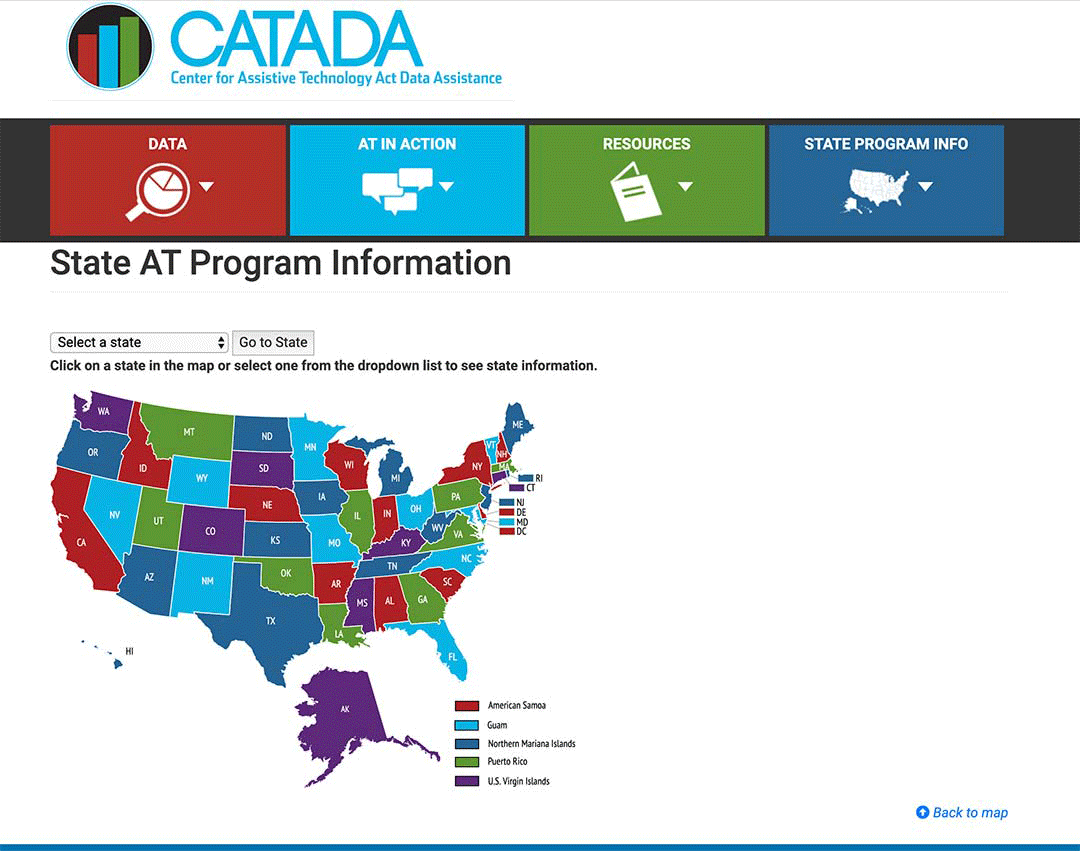
How to find HCBS programs, waivers and 1915 waivers in your state ?
If you would like to check the HCBS Waivers, 1915 Waivers, HCBS Programs and the Money Follows The Person Programs for seniors which are run in your state, I have an article with a list of the programs and waivers in each state, along with links to the appropriate websites. The article also lists all the PACE programs (Programs of All-inclusive Care for the Elderly) in each state –“Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”
How do you acquire DME with Medicaid and state waivers and HCBS programs ?
- a doctor, or therapist, need to write a medical justification letter for you, which states that your equipment is medically necessary
- the medical justification letter then needs to be given to a Medicaid-approved DME supplier
- the Medicaid-approved supplier will then fill out what is called a Prior Approval Application
- the Prior Approval document is delivered to the Medicaid state office for approval or refusal
- if your claim doesn’t succeed, you will be notified by Medicaid as to why, and as to how you may appeal their decision
- if your claim was successful, the supplier will have it delivered to you
What if your revenue is too high to qualify for Medicaid ?
The Spend Down Program
Spend Down programs help the program participants to qualify for Medicaid coverage.
The program participants can make deductions of certain expenses and some debts and loans depending on the method they are using to “Spend Down”
There are two methods –
- Income Spend Down
- Asset Spend Down
Should you wish to find out more, I have an article where I explain who can qualify for Spend Down, the expenses you can deduct on a Spend Down, and how you know if you qualify – What is Spend Down ?
To find your State Medicaid State Agency
If you want to discuss things, or to email someone, you can contact your state Medicaid Agency here.
Step 1 –
Click the link to Medicaid.gov and look for the section that I have outlined in red.
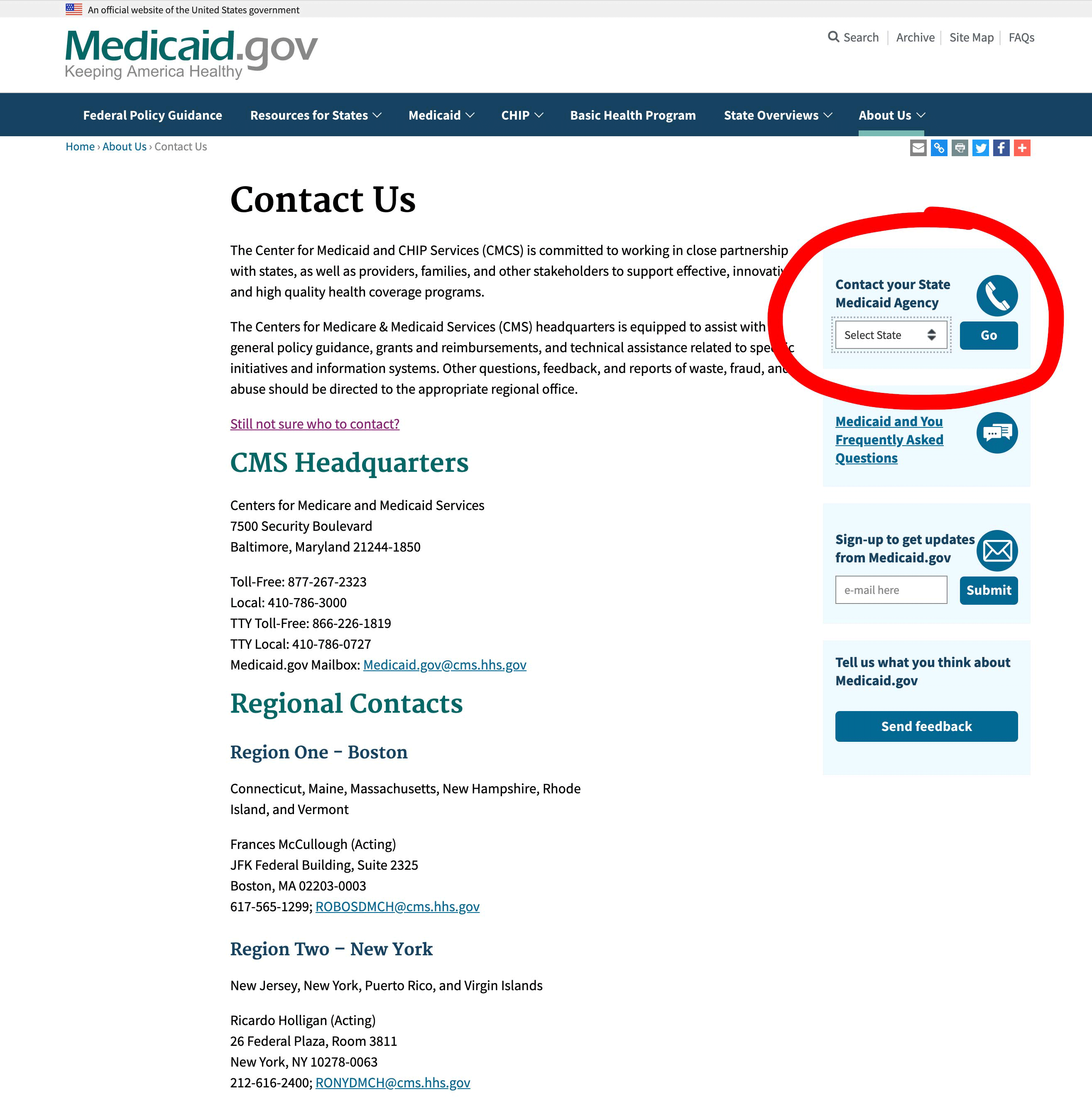
Step 2 –
Select your state and click on the button they have marked “GO” – it will take you to your State Medicaid Agency with all their contact info.
Other state assistance for finding hospital beds for the elderly
State Assistive Technology Programs
The government gives all states across the US have what is called a State Assistive Technology Grant.
With this grant, each state sets up their own State Assistive Technology Program, to improve access to assistive devices in the home, primarily for the elderly and the disabled.
State Assistive Technology Programs will usually have –
- an online equipment and devices exchange where people can post used assistive devices and medical equipment for donation, sale or exchange – any state resident can just register and participate
- a main website where you can keep abreast of their activities and ask about how to get access to free equipment
- reuse, recycling and refurbishment programs which are run by the state program, sometimes in partnership with local community groups and non-profits, to provide free or low cost equipment for the disabled and the elderly
- loan closets are also often a part of their projects, and are either long term or short term, or both
Assistive Technology Programs will also have to register people who are eligible and need help, and will then contact them when specific equipment which they need becomes available.
Your State Assistive Technology Program website will have the information on the different services.
To see what projects are in your state, click here.
Follow the steps below to see the projects in your state
Step 1/
Pick your state on the map or the drop-down menu, and click on “Go to state”
– I chose Florida for this example
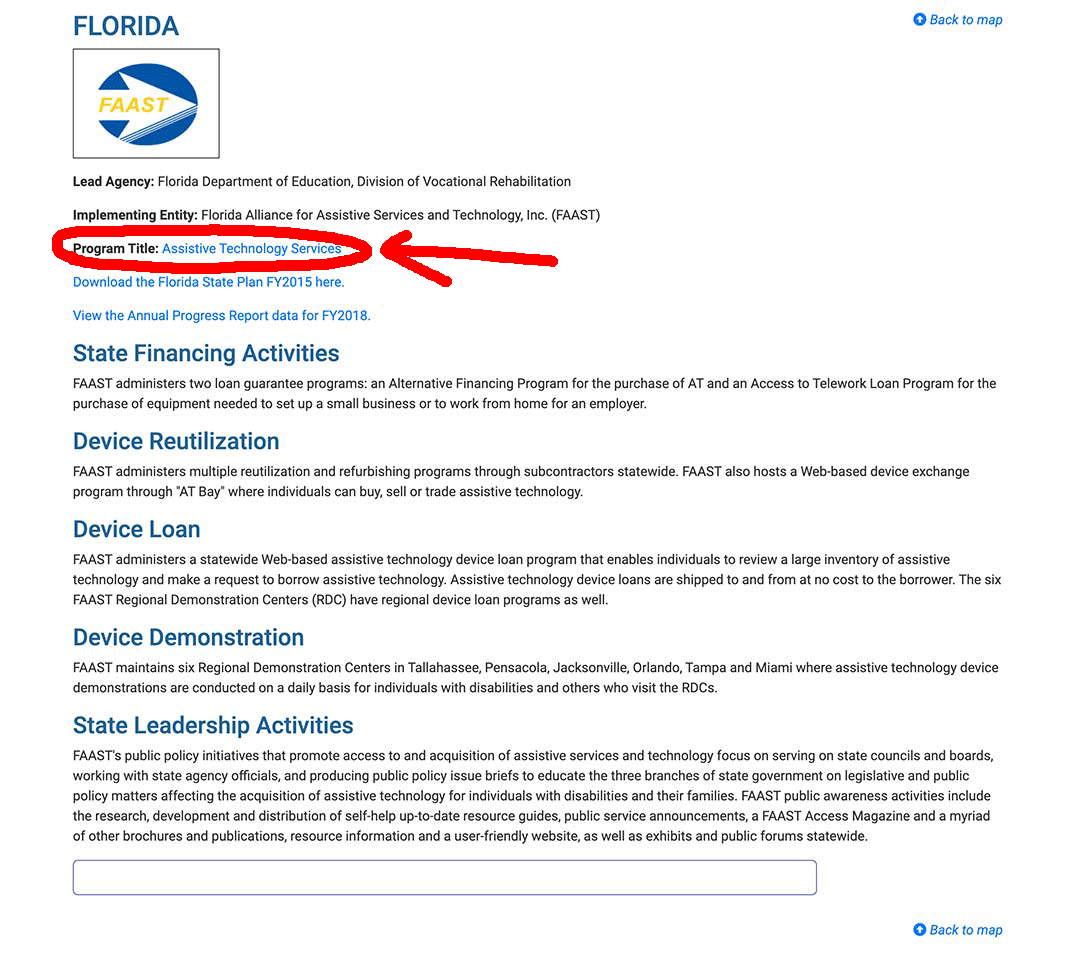
Step 2/
Click on the link “Program Title” – for my example I outlined it in red.
Step 3/
The AT Program state website will come up, and you can register, or use their contact info .
State Financial Assistance Programs
As well as the programs we have looked at, some states have non-Medicaid programs which help the elderly and the disabled to maintain their independence in their homes with financial assistance.
State Financial Assistance Programs will help to purchase assistive devices, safety equipment, durable medical equipment, as well as necessary home modifications.
The participants may get grants or loans, or both.
Your local Area Agencies on Aging should be able to advise on programs for the elderly, and in particular if there is one in your state.
Free hospital beds for the elderly
There are a number of ways of finding hospital beds for free –
- Medicare isn’t free, but if you are enrolled in Medicare Part B, and you qualify under their guidelines, Medicare will pay 80% of the medicare approved price of a hospital bed for home use bought from a Medicare-enrolled DME supplier
- with Medicaid, as I outlined above, you have HCBS programs, waivers, and 1915 waivers, which, if you are accepted into such a program, will very often pay for “medically necessary” equipment, if it will improve, or maintain, your condition
- loan closets, or lending libraries, will make short term, long term or indefinite loans of medical equipment, for people in financial need in their area – these may be run by State AT Programs, or private nonprofits
- state assistive technology programs also often have free gifted equipment posted available to all users on their online exchange websites – I have often seen hospital beds for free, or at a very low cost on these exchanges
- on eBay or Craigslist, you can find donated equipment
- non-profit “reuse” and “refurbishing” centers will all have medical equipment such as hospital beds for sale at a very low cost, or for free to those in financial need – some work with the State AT Programs, but not always, so just check in with your local Area Agency on Aging, as they will, should know of any centers in your area
- local churches may run charities which help those in need with free medical equipment
Do use your local Area Agency on Aging.
An Agency on Aging should be able to tell you what different groups are working to help the elderly in your area, which includes where reuse centers, loan closets and community groups are near to you.
Summary
You can get an adjustable hospital bed covered 80% by Original Medicare, but it will only be a basic model that fulfills your medical needs, and you will have to follow the right procedure for it to be covered as fully as possible.
If Medicare agrees that your claim meets their criteria, you will still have to pay, at least, the co-pay, which is 20% of the Medicare approved price of the bed.
If you wish to have an upgraded model, you can arrange to pay the difference yourself.
Don’t forget, when talking with the DME supplier, to make sure that you ask if they are a Participating Supplier who accepts “assignment”.
If Medicare doesn’t cover your claim, you may still be able to get help through a state HCBS program, or waiver, or if you are a veteran you can look at the different pensions which will help with this.
There are also non-Medicaid state plans which exist to help the elderly maintain their independence in their own home, for which you may qualify if the bed is critical to you maintaining your independence. You can find out about these at your local Area Agency on Aging offices – here is a link to the National Association of Area Agencies on Aging, which has a locator for local agencies – click here.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.