Sometimes the only option, for making a part of the home safe for our elderly parents, is to make modifications to the actual rooms, and the bathroom is probably the room which needs the most work. This can be a simple grab bar or a walk in bathtub. But whatever the solution, we still have to find out how to pay for it.
Original Medicare Part B does not typically cover bathroom modifications, although Medicare Advantage plans may offer bathroom modifications which help beneficiaries who suffer with some chronic conditions.
Almost all home modifications will not be covered by Medicare Part B.
Medicare Part B typically only covers durable medical equipment for use in the home which it considers to be “medically necessary”, and unfortunately equipment for the bathroom is for the most part considered to be for comfort, and modifications are seen as not primarily medical in nature.
In the very rare instances that Medicare will cover the cost of bathroom modifications i.e. walk in bathtubs, Medicare has to be convinced that it really is a “medical necessity” – to prove this a medical diagnosis a proof of need is required, and a prescription of “medical necessity” from a physician which demonstrates –
- why the patient cannot live without the modifications – the necessity
- what it is that is needed from the required equipment, or modification
In addition to the above, Medicare Part B also requires that it can be reasonably expected that the equipment or modification will either maintain the patient’s condition or give rise to an improvement in their condition.
Just because a person has a prescription of “medical necessity”, a diagnosis and a statement saying it will either improve, or maintain the condition of their health, it isn’t a guarantee that medicare will give the coverage
And on top of that, the claimant will also have to pay up front hoping that Medicare will agree, and reimburse them to some extent.
Medicare Advantage Plans, or Medicare Part C, can offer benefits which are for chronic illnesses, and some may be for bathroom modifications. More on this later.
Contents Overview & Quicklinks
Does Medicare cover shower chairs ?
Does Medicare cover bathroom equipment ?
Does Medicare cover walk-in showers ?
Does Medicare cover wheelchairs ?
What medical supplies does Medicare cover ?
What equipment does Medicare pay for ?
Does Medicare Advantage cover bathroom modifications ?
Local Medicare-enrolled DME Supplier near you
List of durable medical equipment typically covered by Medicare
How to get coverage from Medicare Part B for durable Medical Equipment ?
What to do once you have a signed prescription ?
Free help with understanding Medicare
Does Medicaid cover home modifications or bathroom equipment ?
Which types of Medicaid programs will most likely allow for bathroom modifications ?
How to find the HCBS programs etc. in your state ?
What’s the procedure for getting DME with Medicaid state waivers and HCBS programs ?
If your income is a bit too high to qualify for Medicaid
State Assistive Technology Programs
Does Medicare cover shower chairs ?
Medicare Part B usually won’t cover shower chairs, as they are not seen as “medically necessary”.
Medicare Part C, or Medicare Advantage Plans, which offers a wider range of benefits than Medicare Part B, in some cases may well offer coverage for a shower chair.
To get coverage for a shower chair for use in the home, your doctor, who must be a Medicare-enrolled physician, has to prescribe a shower chair for you, to document why it is “medically necessary” and to show that it is going to help you with your care of a diagnosed medical condition.
To find out more about the different documents, the diagnosis, the guidelines, and letter of medical necessity for a shower chair, you can read my article “Does Medicare Cover Shower Chairs”.
Does Medicare cover bathroom equipment ?
As I said above, Medicare coverage extends to items which it sees as “medically necessary”, but not too many safety items which it sees as comfort items or, “not primarily medical in nature”.
By the way, I am not plucking the term “not primarily medical in nature” out of thin air, it is one of the terms that Medicare uses on its statements of coverage, as a reason for denial.
A large part of what we would see as safety equipment helping the elderly to continue to live independently in their homes, is not covered by Original Medicare.
Medicare Part B does not typically cover any of the following –
- grab bars
- raised toilet seats
- transfer seats
- bath lifts (these are seats which rise up and down within the bathtub)
- floor to ceiling poles
- shower chairs
- bath chairs
- toilet safety frames
Fortunately, some medical equipment designed for the elderly with mobility issues is covered (as long as it is proven to be “medically necessary”), and can useful in the bathroom for avoiding falls –
- crutches
- walkers
- bedside commodes
- patient lifts
Bedside commodes, with adjustable legs (often called a 3 in 1 or All in One), can be used as –
- a raised toilet seat
- a shower chair if they are waterproof
- a safety frame for the toilet
- a safety frame or chair in front of a sink
- or as a chair for a sponge bath in the bathroom
Walkers which are waterproof –
- can be used as an aid to standing in the shower, so long as they are a waterproof model
- any type of walker can be used as a safety rail in front of the sink or mirror
- as an aid to sitting down on, and getting up from the toilet
Patient lifts which are mechanical and which are covered for people who cannot leave their beds (there are strict guidelines) can in a lot of cases be used to help a person wash themselves in a shower or tub.
Does Medicare cover walk in showers ?
Typically, Medicare Part B doesn’t cover bathroom safety equipment or modifications as I noted earlier, and unfortunately walk in showers fall into this area.
It is considered to be a comfort item and “not primarily medical in nature”.
But as I have also noted if you can prove that it is unconditionally “medically necessary”, with a prescription certifying this from a Medicare-enrolled doctor, a diagnosis with “proof of need” that supports this, lots of supporting evidence of why you can’t live without it, evidence of why this particular walk in shower will do what you need, and that it can be reasonably expected that the shower will either maintain or improve your condition, then Medicare may agree to help cover.
Or you could wait until the fall of 2020 to see which Medicare Advantage plans may be offering to cover modifications or walk in bathtubs, and switch from Medicare Part B to that plan.
Does Medicare cover wheelchairs ?
Medicare Part B covers wheelchairs and power-operated vehicles for use in the home when a Medicare-enrolled physician –
“submits a written order stating that you have a medical need for a wheelchair or scooter for use in your home.”
Source – https://www.medicare.gov/Pubs/pdf/11046-Medicare-Wheelchair-Scooter.pdf
The information above comes from the Medicare Wheelchair and Scooter Benefit PDF.
What medical supplies does Medicare pay for ?
Medicare Part B covers specific durable items for use in the home that are proven to be “medically necessary”, and prescribed by a Medicare-enrolled physician.
The medical items it covers are called “durable medical equipment”.
Disposable medical supplies are not generally covered, but any disposable supplies which are needed for use in conjunction with durable medical equipment will typically be covered.
Disposable medical supplies which Medicare Part B does not cover include items such as diapers, bandages, face masks, pressure leotards, support hose, surgical leggings, disposable sheets and bags, fabric supports and incontinence pads.
Blood sugar strips and certain catheters are disposable, they may be covered by Medicare, if they are needed to treat long term medical conditions.
If you receive the Home Health Care Benefit, Medicare will cover some disposable medical supplies needed for your care.
What equipment does Medicare pay for ?
Original Medicare Part B covers 80% of the Medicare-approved price of durable medical equipment, or DME, for use in the home, when it is “medically necessary” as prescribed by a doctor, or treating provider, and bought or rented from a Medicare-approved supplier.
You will find a long list I have put together of durable medical equipment typically covered by Medicare Part B which you can jump on down to here.
Do bear in mind that Medicare Part B will only cover equipment for use in the home if you qualify under their guidelines.
Just because you decide you need a piece of equipment doesn’t mean they will give it coverage.
For Original Medicare, durable medical equipment should fulfill the following criteria :-
- Durable (can withstand repeated use)Used for a medical reason
- Not usually useful to someone who isn’t sick or injured
- Used in your home
- Generally has an expected lifetime of at least 3 years
Source: Medicare.gov website – here
In its own literature, Original Medicare often lists typical examples of durable medical equipment which it will cover as wheelchairs, crutches and walkers.
Typically, the beneficiary, will be responsible for paying a coinsurance payment of 20% of the Medicare-approved price any piece of durable medical equipment that Medicare may cover, plus if it applies, their deductible.
Does Medicare Advantage cover bathroom modifications ?
Medicare Advantage Plans or, Medicare Part C, are plans which are run by private companies which have been contracted to provide, at a minimum, the same services as Original Medicare.
Medicare Advantage Plans have extra to make them more competitive with Original Medicare.
For those Medicare Advantage Plans, new benefits have been allowed for those policies, as of the end of 2020.
In 2019, the Centers for Medicare & Medicaid released their plans to increase the competitiveness and coverage of Medicare Advantage and Medicare Part D plans.
Beginning in 2019, Medicare Advantage plans can now offer supplemental benefits that are not covered under Medicare Parts A or B, if they diagnose, compensate for physical impairments, diminish the impact of injuries or health conditions, and/or reduce avoidable emergency room utilization.
Source: “CMS finalizes Medicare Advantage and Part D payment and policy updates to maximize competition and coverage” April 1, 2019. You can read this on the CMS.gov website here.
Some Medicare Advantage plans now offer new benefits for bathroom safety equipment, and bathroom modification.
Local Medicare-enrolled DME Supplier near you
You can use this link to find a Medicare-approved supplier who is local to you – Medicare.gov
List of Durable Medical Equipment typically covered by Medicare
If you don’t find the equipment you are looking for in my list of Original Medicare Part B covered DME’s below, you can use this link to Medicare.gov
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
How to get coverage from Medicare Part B for Durable Medical Equipment ?
To be eligible for Original Medicare Part B coverage for durable medical equipment for “use in the home” –
- you need to be enrolled in Medicare Part B
- you need a signed prescription from your Medicare-enrolled doctor which certifies that the equipment is “medically necessary”
- you need to acquire the DME from a Medicare-enrolled supplier
What counts as “living at home” for Original Medicare ?
For the purposes of Original Medicare, “living at home” can be –
- living in your own home
- living in the family home
- living in the community, such as assisted living
What do you do once you have a signed prescription ?
After you have received your prescription –
- you need to choose a Medicare-enrolled DME supplier
- you should only use a Medicare-enrolled “participating supplier who accepts “assignment’ – as this means you will pay the least amount possible for your equipment
- you will then pick out the DME which corresponds to your prescription with the supplier
- make sure you have completed all the requisite paperwork for Medicare with the supplier
- if your supplier accepts assignment (the Medicare-approved price) then you will typically be responsible for 20% of the cost – this is your coinsurance
- if your supplier does not accept assignment, you may have to pay everything upfront, and the supplier will send the claim on your behalf to Medicare and you will wait to be reimbursed 80% of the Medicare-approved price, by Medicare
- if a supplier who does not accept assignment does not believe that Medicare will reimburse your claim, they must notify you in advance with an Advance Beneficiary notice
Just to be clear –
If you are acquiring the DME from a Medicare-enrolled “participating” supplier who accepts assignment, you will have only the Medicare 20% coinsurance payment of the Medicare-approved price of the DME to pay, and your policy deductible if it applies.
Free help with understanding Medicare
SHIP – State Health Insurance Assistance Programs
Free guidance services for Medicare, Medicaid and Medigap in all states in the US from the State Health Insurance Assistance Program
The counseling is given over the phone in most cases.
Read this very short piece to find your SHIP – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Does Medicaid cover home modifications ?
Without going into a complex description of how Medicaid is funded, it will suffice to say that it is funded partly federally, and partly by each state.
For this reason, a state will have a large say in the way in which different Medicaid based programs and services are funded.
This is particularly true in the case of different programs and services which states will offer for home based care, and services relating to, or leading to, the setting up of care in the home, and for moving the provision of care away from nursing home facilities, and back into the home.
Medicaid will frequently agree to waive eligibility requirements for certain programs, allowing the state to extend their reach to demographics which might otherwise be neglected.
A program for which Medicaid agrees to waive requirements is known as a “waiver”.
Care in the home – Medicaid and state programs outside of institutions
“Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers” are the names given to the programs which are set up to care for individuals in their homes and in the community.
The primary goal of such programs is to assist the participants in maintaining their independence in both their homes.
“Home medical equipment” which is medically necessary for the participants, will be covered by HCBS waivers and programs, and regularly up to 100% of the cost.
Your State Medicaid Agency should be able to give you any information on what is available and the eligibility requirements for programs- you can contact them here.
To find out more about HCBS programs, or waivers, check here on Medicare.gov –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
For these programs, the term “home” means –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
Which types of Medicaid programs will most likely allow for bathroom modifications ?
Some HCBS programs, waivers and 1915 waivers allow for the beneficiaries to have a large say in how their allocated budget is spent.
These are called either “Consumer Direction”or “Self Direction”.
Such programs are set up so that the beneficiary, along with the help of a financial advisor, can manage their resources to cover their needs.
If the equipment or home modification is medically necessary for the participant to maintain their independence, and it is within their budget, there is a very good chance it will be allowed.
To find out more about Medicaid Self Direction click here.
The Medicaid program “Money Follows The Person”
To transition elderly adults living in nursing homes back to their own homes Medicaid set up Money Follows The Person.
Today, Medicaid provides funding to the states to do the same, either by building a new “Money Follows The Person” program, or by adapting a suitable program which already exists.
Money Follows The Person programs will often, if it is critical to a person moving back into their home, pay for remodeling rooms, improve lighting, or building ramps as well as buying any medically necessary DME.
How to find the HCBS programs, waivers and 1915 waivers with their eligibility criteria in your state
I have a complete guide to the HCBS programs and waivers offered by each state for seniors, along with links to all the different program websites here – “Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”.
What’s the procedure for getting DME with Medicaid state waivers and HBSC programs ?
Step 1
– the doctor, or therapist, has to provide a medical justification letter, stating it is medically necessary
Step 2
– find a Medicaid-approved DME supplier, and give them the medical justification letter
Step 3
– the Medicaid-approved supplier fills out a Prior Approval Application form for Medicaid
Step 4
– the Prior Approval Application is sent to the Medicaid State Office
Step 5
– if you are unsuccessful you will be contacted and given the reasons as to why, as well as advice on how to make an appeal
Step 6
– if approved, you will receive the DME
If your income is a bit too high to qualify for Medicaid
Spend Down Programs
Spend Down programs have been devised by Medicaid to help to reduce a person’s income level, asset + income level, so that the person may become eligible for Medicaid coverage.
There are two methods for “spending down” –
- Income Spend Down
- Asset Spend Down
With both methods the program participants are allowed to deduct, from their income certain medical expenses, and with the Asset Spend Down certain loan payments, and even debt repayments are also permitted, so that the participant’s income and assets drop below the Medicaid limit.
You can find my article outlining who can qualify for Spend Down, the expenses they can deduct and how you know if you qualify, here – What is Spend Down ?
To find your State Medicaid State Agency
If you want to discuss things, or to email someone, you can contact your state Medicaid Agency here.
Step 1 –
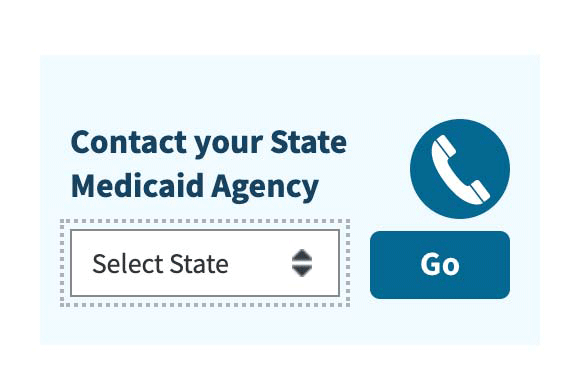
Click the link to Medicaid.gov and look for the section that I have outlined in red.
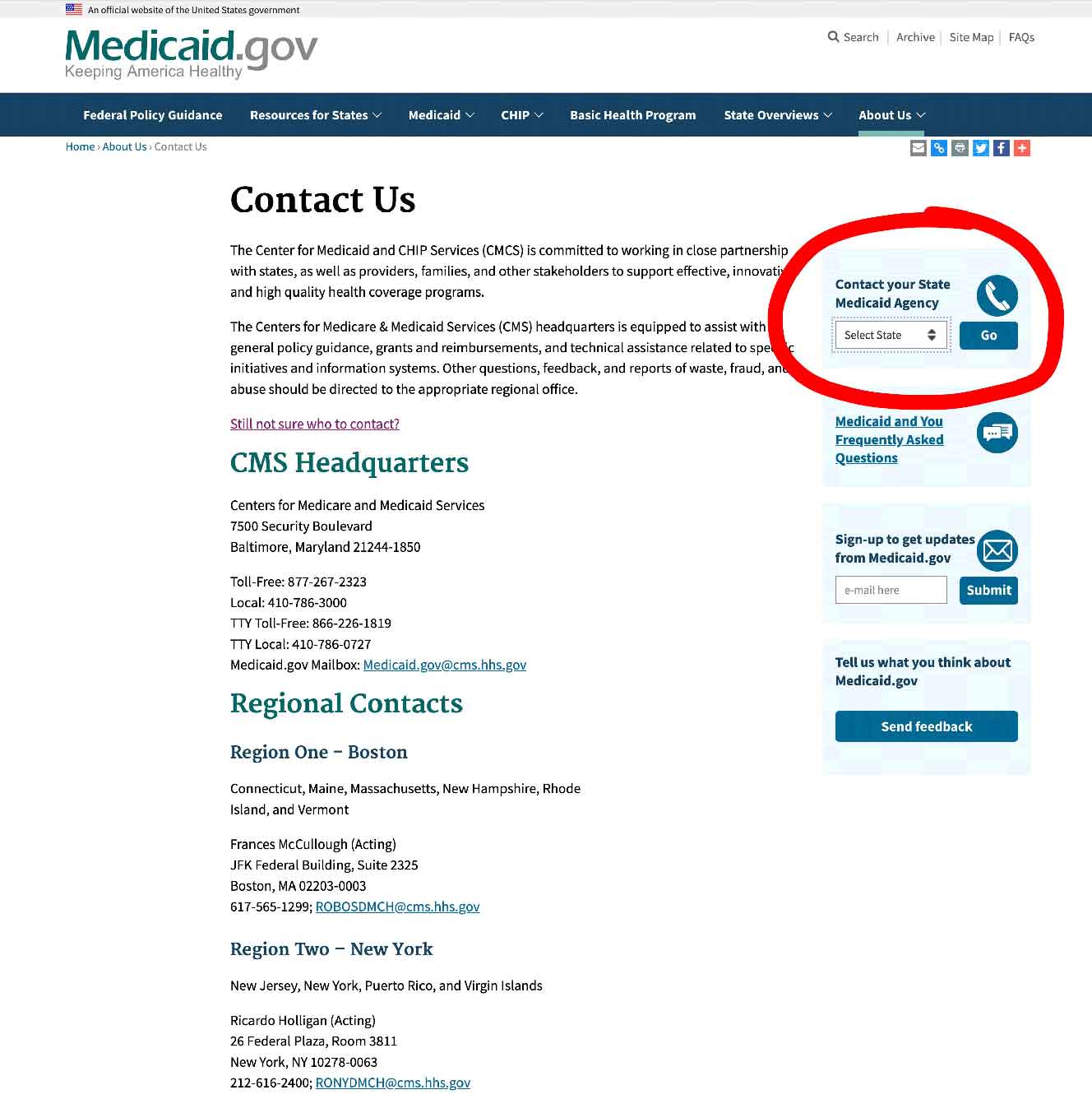
Step 2 –
Select your state and click on the button they have marked “GO” – it will take you to your State Medicaid Agency with all their contact info.
State Assistive Technology Programs
Each state has a State Assistive Technology Program.
The goal such projects is to improve access to assistive devices in the home, primarily for the elderly and the disabled.
The term “assistive technology device” is very much similar “durable medical equipment”
The State Assistive Technology Programs typically have –
- a website where state residents can post notices for assistive devices/durable medical equipment for donation, exchange or for sale – an “online exchange” – all you have to do is register online, and you are good to go
- a main State Assistive Technology Program website which will coordinate the services, register people in need, handle the administration and act as a communications hub to the project as a whole
- programs for reuse and recycling which are often run by non-profits and community groups which have partnered with the State Assistive Technology Program, to provide free, or very cheap “gently used” devices and equipment for the disabled, the elderly
- some State Assistive Technology Programs will also have short and long term loan closets as part of their programs
At your State Assistive Technology Program website, you can find out more.
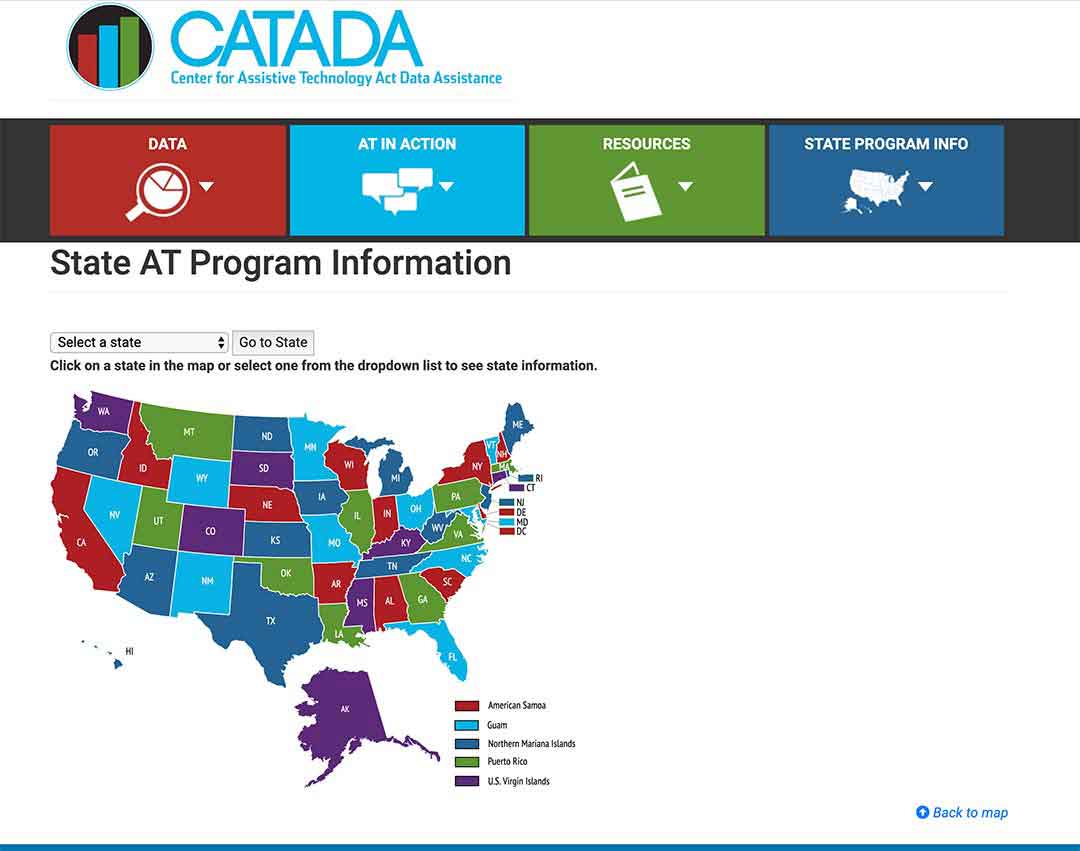
To see what programs are in your state click here
Step 1/
Pick your state on the map or the drop-down menu, and click on “Go to state”
– I chose Florida for this example
Step 2/
Click on the link “Program Title” – for my example, I outlined it in red.
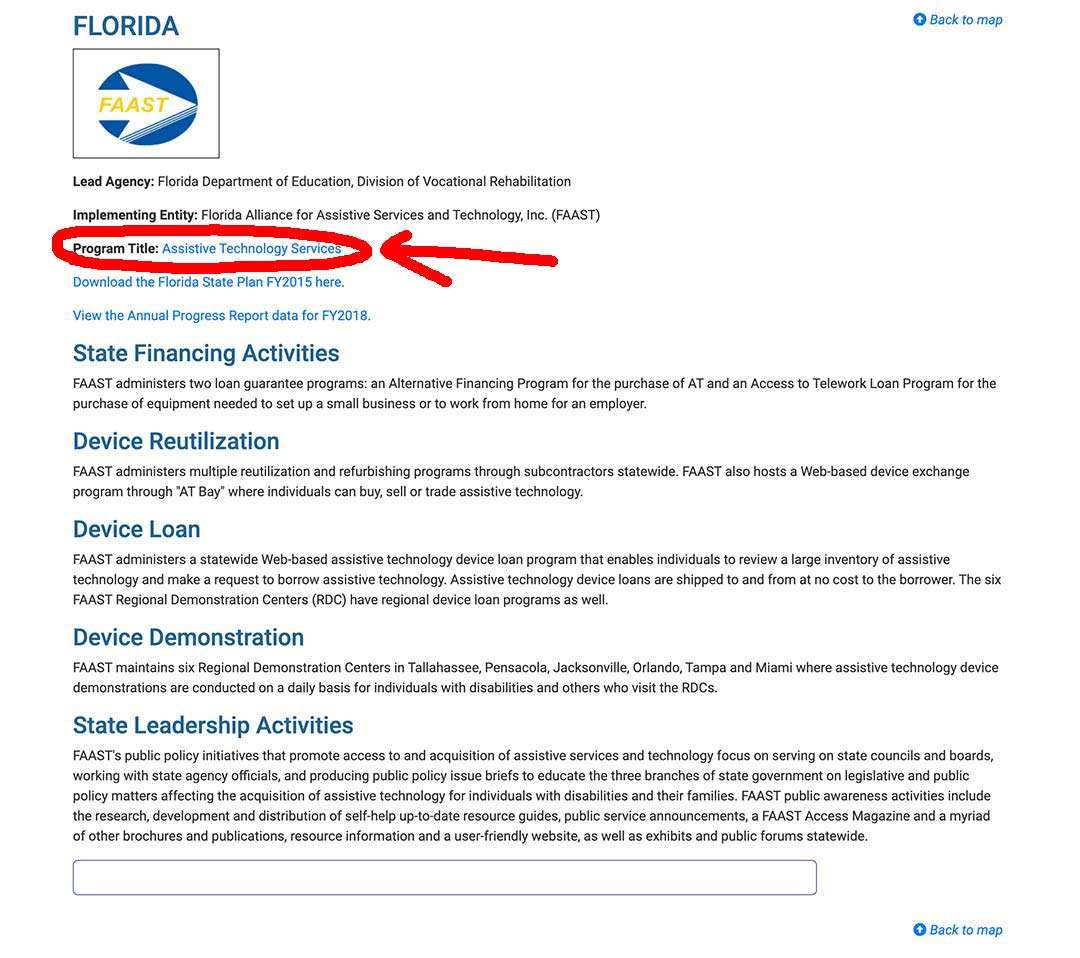
Step 3/
The AT Program state website will come up, and you can sign up, or use their contact info .
Grants for home modifications for the elderly
State Financial Assistance Programs
Some states have non-Medicaid State Financial Assistance Programs which assist the elderly and the disabled with grants and loans, to pay for assistive devices, durable medical equipment, and home modifications, which will allow them to continue living independently in their own homes.
These programs can also be called Nursing Home Diversion Programs – the goal being to maintain an elderly person’s independence in their home rather than moving them into a nursing home.
To find whether your state has a State Financial Assistance Program for the elderly and disabled, check with your local Area Agency on Aging.
USDA Rural development Section 504 Home Repair program
For elderly adults living in rural areas, it is possible to get a grant for home modifications under certain circumstances.
Loans to low-income homeowners to “repair, improve or modernize their homes or grants to elderly very-low-income homeowners to remove health and safety hazards.” are allowed by the USDA – source USDA.GOV
The grant is a maximum of $7500.00.
If the house is resold within three years of receipt of the grant, the grant must be repaid.
To be eligible for the Home Repair program grant –
- you must be the homeowner
- you must be 62 yrs or over
- you must have a family income of less than 50% of the local average income
- you must be unable to repay a home repair loan
Applications for the grant are accepted year round at your local Rural Development office here
You can talk to a local USDA Home loan specialist for advice here.
Veterans-Direct HCBS
This program is meant for veterans who are at risk of losing their independence and having to move into a nursing home.
The veterans are given a budget which they are allowed to use to purchase what they need to maintain their independence, i.e. the services they require.
The budget can also be used to pay for home modifications, such as –
- grab bars
- lighting
- wheelchair ramps
- bathroom equipment
Low Income Home Energy Assistance Program
This program provides assistance to eligible low income households with “their heating and cooling energy costs, bill payment assistance, energy crisis assistance, weatherization and energy related repairs.”
Source: https://www.benefits.gov/benefit/623
The assistance can be for home modifications related to weatherization or energy-related repairs.
You can find out about eligibility and how to apply on the link above.
Weatherization Assistance Program
The elderly can get assistance with modifications to improve a home’s energy efficiency.
The program works on a state level.
On the website for the program you can find a locator tool here to contact you state administrator.
Nonprofits offering services
There are a number of nonprofit organizations which offer their help with building modifications to the elderly and the disabled.
One such organization working across the US is Rebuilding Together.
Rebuilding together has affiliates across the US, and they will come and volunteer their time and skills to restore or modify homes for those in need.
You can find out if there is an affiliate group near you by using their locator tool here on their website.
To find out what other nonprofits are available near you, contact your local Area Agency on Aging.
To Summarize
Typically, Medicare Part B will not cover any home modifications -in very rare cases they may do so if it can be proved that it is medically necessary and will either maintain or improve the health condition of the beneficiary in question.
But as of 2020 Medicare Advantage plans will be allowed to offer extra benefits, and it is widely assumed that some plans will include bathroom modifications as a benefit, so you may well want to consider switching from Medicare Part B to a private Medicare Advantage plan in your area if they are offering such a benefit.
For those who qualify for Medicaid, their HCBS waivers will often allow for home modifications and bathroom equipment, and more specifically those which are called “Self Direction” or “Consumer Direction”.
If you can’t get free modifications, don’t forget to look on your State Assisted Technology Program website or online exchange, as you may at least be able to get the equipment for free or very cheaply.
And finally, if you live in a rural area, and have a very low income, then you can look at the USDA Rural development Section 504 Home Repair program.
Good luck and I hope it helps.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.

