Every day, I help my mom go through her little routine of exercises to keep her back strong, and to make sure her hip replacement doesn’t do anything it shouldn’t.
Staying healthy is going to be the number priority for all of our elderly loved ones. There are lots of ways of doing this, from eating well, to joining exercise groups and buying home exercise equipment. It all comes at a financial cost, and we are left looking for ways to pay.
Does Medicare cover exercise equipment ? Original Medicare does not cover any exercise equipment, as it is not primarily medical in nature.
Some Medicare Advantage plans may give cover for exercise programs.
You may be able to get funding for exercise equipment from Medicaid, and or other state funding sources.
Contents Overview & Quicklinks
Original Medicare coverage for Physical and Occupational Therapy
Will Medicare cover your bathroom equipment ?
How often does Medicare pay for a walker or DME ?
How do you qualify for Medicare coverage for DME ?
So, now you have a prescription from a Medicare-enrolled doctor, what do you do ?
Will Medicare purchase or rent my DME ?
Locate Medicare-enrolled DME Supplier near you ?
Do Medicare Advantage Plans cover exercise equipment ?
List of Durable Medical Equipment typically covered by Medicare
List of Durable Medical Equipment not typically covered by Medicare
Get free assistance with understanding Medicare
Will Medicaid cover bathroom safety equipment ?
Medicaid and state programs and waivers for in the home care services
With certain programs and waivers, there may be a broader interpretation of what qualifies as a DME
How to find the HCBS programs, waivers and 1915 waivers in your state ?
How to get DME with Medicaid and state waivers and HCBS programs ?
Original Medicare coverage for Physical and Occupational Therapy
Original Medicare Part B covers physiotherapy and occupational therapy, where it –
- is prescribed as “medically necessary” by a Medicare approved physician
- the therapist providing the treatment must be doing so on an outpatient basis
- the therapist must be Medicare-certified
- the therapy must be regularly reviewed by the prescribing physician
***As with equipment, you will need to make sure that therapists charge the Medicare-approved amount.
Medicare will typically pay 80% of the Medicare-approved fee, and the patient covers the remaining 20%, plus their deductible if it applies.
If you have a Medicare Advantage Plan, you may discover that you have coverage for exercise plans and gyms, but you will need to ask your provider.
For those of you who have been a caregiver for a while, it won’t be a surprise to discover that if a piece of equipment is not considered by Medicare to be “medically necessary”, or “not primarily medical in nature”, Medicare typically will not cover it.
I am going to take a look at some medical and safety equipment to broadly outline –
- what Medicare will and won’t typically cover
- how to get Medicare coverage when it is available
- how to not make mistakes with Medicare
- how to get free Medicare guidance in your state with a counselor
Medicare Free Supplies
Medicare does not have any “free” supplies, but on certain supplies and equipment Medicare will cover up to 80% of the cost, if you are enrolled in Medicare Part B and you qualify under their guidelines.
Medicare does not cover supplies which are not reusable, such as gauze or bandages, unless they are being used in conjunction with a piece of medical equipment which does qualify.
Medicare does cover some medical supplies as Durable Medical Equipment.
Durable Medical Equipment
What is it ?
Durable Medical Equipment, or DME, can be described as medical equipment which can be used in the home, and which will withstand repeated use over a sustained period of time.
For Original Medicare, “Durable Medical Equipment” includes items such as –
- wheelchairs
- bedside commodes
- walkers
- hospital beds
Durable Medical Equipment is covered by Original Medicare Part B, for use in the home, when it is prescribed as medically necessary –
- by a Medicare-enrolled Physician
or by a
- “treating provider (like a nurse practitioner, physician assistant, or clinical nurse specialist)”
–in either case this is done by filling out an order, and may demand extra documentation of the medical necessity of the equipment in certain cases.
Source : https://www.medicare.gov/Pubs/pdf/11045-Medicare-Coverage-of-DME.PDF
The equipment must also be purchased, or rented, from a Medicare-enrolled supplier to qualify for coverage.
Medical equipment used in skilled nursing facilities, including DME for short term stays, is covered by Original Medicare Part A (hospital care).
For equipment to make it onto the Medicare list of Durable Medical Equipment which may be covered, it must fulfill the following criteria –
- it must hold up to sustained use over a long period of time – durable
- it can only be used for medical reasons – not for comfort
- it’s got to be useful to a person who is sick, and hardly of use to a person who is not
- it must be used primarily in the home
- it must be expected to function properly for a minimum of 3 years
Will Medicare cover your bathroom equipment ?
The bathroom is likely the room considered to have the greatest number of risks for the elderly, and it has just about the largest range of safety equipment available to it.
Sadly, Medicare Part B is not going to help much.
Medicare Part B will not cover what it considers to be comfort items, and that includes all the following –
- grab bars
- raised toilet seats
- bath lifts
- shower chairs
- bath chairs
- transfer seats
- toilet safety frames
Original Medicare Part B will though typically cover crutches, walkers and bedside commodes, if they are “medically necessary”, and these pieces of equipment can help in the bathroom to reduce the risk of falling, and to lend stability to those who have mobility and strength issues.
For those with Medicare Advantage plans, as of the fall of 2020, some plans may cover some bathroom safety equipment due to the changes in extra benefits covered.
To find out which Advantage plans will cover some bathroom safety equipment, you will have to consult with an insurance agent in your state.
I have a long article, with 50 plus safety tips, that I have learned over the 11 years that I have looked after my mom and dad. These are both practical tips, and some suggestions for bathroom safety equipment that you may find helpful. You can read the article here.
If you are looking for suggestions and advice on how to make bathing easier for your parent, especially if you are assisting them, then I have another article discussing ways I have found useful to make it a more comfortable and dignified experience for all parties – that one is here.
How often does Medicare pay for a walker, or DME ?
Original Medicare Part B will replace DME that you rent, or own, if it’s –
- worn out through use
- been in your possession for its entire lifetime
- it must be so worn out that it can’t be fixed
- five years is the minimum period considered to be a lifetime for an item
- the lifetime can vary depending on the type of equipment
In the case of a walker which is worn out, Medicare Part B will typically replace it every five years, so long as it has always been in your possession, and it is beyond repair.
If an item is worn out prior to the end of it considered lifetime, Medicare will pay to repair it, that is, unless the repair is more costly than a replacement item.
If you need to replace a worn out item, you will have to go through the process of getting a prescription from a Medicare-enrolled doctor stating that your walker is medically necessary.
The process is pretty much the same for all replacement items, apart from those which require prior approval.
How do you qualify for Medicare coverage of DME ?
To be able to qualify for Medicare coverage of DME’s “for use in the home” under Original medicare Part B, you –
- must be enrolled in Medicare Part B
- must get a signed prescription from your Medicare-enrolled doctor stating that your item is “medically necessary”
- need to be purchasing the equipment through a supplier who is a Medicare-enrolled supplier
To qualify for “home use” –
You must be –
- living in your own home
- living in the family home
- living in the community, such as assisted living
So now you have a prescription from a Medicare-enrolled doctor, what do you do ?
Armed with your prescription for your equipment, you –
- find and visit a Medicare-enrolled DME supplier
- always use a Medicare-enrolled supplier
- for the best possible coverage from Medicare Part B, you must make sure that the supplier is a Medicare-enrolled “participating” supplier who accepts “assignment”
- Medicare gives coverage to only the basic models of any equipment, so the range of equipment your prescription will purchase won’t be that large
- for certain equipment you may be allowed to upgrade you, but you will pay the difference between the price of the Medicare-approved model and the upgrade, and it isn’t always possible
- choose the model you like from the range of equipment that you have been prescribed
- it’s time to do any necessary paperwork for Medicare and for the supplier
Medicare part B, typically provides cover for 80% of the Medicare-approved price for DME, because you have a prescription from a Medicare-approved doctor, and because you purchased your item from a Medicare-enrolled supplier.
If you use a Medicare-enrolled “participating” supplier who accepts assignment, you will then, typically, pay your Medicare 20% co-payment of the Medicare-approved price for your equipment, plus your deductible if it applies.
Always use, a Medicare-enrolled “participating” supplier who accepts assignment, if you don’t, you may have to pay a lot more.
Will Medicare purchase or rent my DME
Medicare both rents and buys equipment outright.
The smaller items are usually purchased and the more important pieces, such as hospital beds, are rented.
If your item is rented from a Medicare-enrolled “participating” supplier who accepts assignment, you will typically pay a monthly 20% co-payment of the Medicare-approved rental price for it, and also, if it applies, your deductible.
Locate a Medicare-enrolled DME Supplier near you
To find a local Medicare supplier, check this here at Medicare.gov
Do Medicare Advantage Plans cover exercise equipment ?
In a Medicare Advantage Plan you are covered for at least the same medical services, supplies and equipment that Medicare Parts A and B cover, and sometimes a few extra services, and this can be exercise programs or gym memberships with certain Advantage plans.
So, generally an Advantage plan will not cover your exercise equipment, but they may cover an exercise program, or gym membership.
You need to contact your Advantage plan provider to find out.
If you are trying to get coverage for any medical equipment which is covered by Medicare, don’t forget that you have to go through your Advantage plan provider’s network, their exact process for buying equipment with coverage, the doctors they work with and their supply network.
Using doctors and suppliers outside your plan’s network will likely lead to a loss of coverage.
List of Durable Medical Equipment typically covered by Medicare
If you don’t find the equipment you are looking for in my list of Medicare covered DME below, you can use this link to Medicare.gov
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
List of Durable Medical Equipment typically not covered by Medicare
Adult Diapers
Air Cleaners
Air Conditioners
Alcohol Swabs
Augmentative Communication Device
Bathroom Aids
Bathtub Lifts
Bathtub Seats
Bed Bath
Bed Boards
Bed Exit Alarms
Bed Sensor Pads
Bed Lifter
Beds – Lounge
Bed Wedges
Blood Glucose Analyzers
Braille Teaching Texts
Caregiver Paging Systems
Catheters – except those which are used for permanent medical conditions where the catheter is considered as a prosthetic
Chair Exit Alarms
Chair Sensor Pads
Communicator
Contact Lenses – Medicare helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens
Dehumidifiers
Dentures
Diathermy Machines
Disposable Bed Protectors
Disposable Sheets
Door Exit Alarms
Easygrip Scissors
Elastic Stockings
Electrical Wound Stimulation
Electrostatic Machines
Elevators
Emesis Basins
Esophageal Dilators
Exercise Machines
Exit Alarm Mat
Eye Glasses – Medicare helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens.
Fall Alarms
Fans
Fabric Supports
Fomentation Device
Grab Bars
Grabbers
Gauze
Hearing Aids
Heat and Massage Foam Cushion Pad
Heating and Cooling Plants
Home Modifications
Humidifiers – not room humidifiers
Incontinence Pads
Injectors (hypodermic jet pressure powered devices for Insulin injection)
Irrigating Kits
Insulin Pens
Massage Equipment
Motion Sensors
Motion Sensor Exit Systems with Pagers
Needles
Oscillating Beds
Over bed Tables
Paraffin Bath Units (if not Portable)
Parallel Bars
Portable Room Heaters
Portable Whirlpool Pumps
Preset Portable Oxygen Units
Pressure Leotards
Pressure Stockings
Pulse Tachometer
Pull String Alarms
Raised Toilet Seats
Ramps
Reading Machines
Reflectance Colorimeters
Sauna Baths
Special TV Close Caption
Speech Teaching Machines
Stair Lifts
Standing Table
Support Hose
Surgical Face Masks
Surgical Leggings
Syringes
Telephone Alert Systems
Television Assistive Listening Devices
Telephone Arms
Toilet Seats
Treadmill Exercisers
Walk in Bathtubs
Wheelchair Lifts
Whirlpool Pumps
White Canes
Wigs
Get free assistance with understanding Medicare
SHIP – State Health Insurance Assistance Programs –
Your SHIP offers free counseling over the phone about Medicare, Medicaid and Medigap.
I have a guide outlining how to find your local SHIP here – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Will Medicaid cover exercise equipment ?
The funding of Medicaid has a rather different structure to that of Medicare – it is funded both on a federal level and a state level.
Medicaid provides guidelines within which the states operate their Medicaid system, but with a lot of room to change things, as each state is putting their own funding in as well.
In each state, Medicaid will agree to waive some requirements for eligibility for different programs, allowing the state to provide care to those who might otherwise have been missed, or lost, by the system.
In such cases, which are many across all the states, programs are known as waivers and each will have specific eligibility requirements, and generally a limited number of places.
Even though the waivers may vary greatly, there are waivers in all states which are specifically to help with care in the home for the elderly and the disabled.
With all these extra programs and waivers across the US, there is a great deal more flexibility and variety as to what can be considered DME, by comparison with Medicare.
Medicaid and state programs and waivers for in home care services
“Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers” are names of the services, and programs, offered to care for individuals in their homes and the community.
The primary focus of these programs is low income families, disabled individuals and the elderly with medical needs.
To read more about HCBS programs, waivers, or 1915 waivers, you can go to Medicaid itself at medicaid.gov –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
HCBS programs, waivers, and 1915 waivers will all pay for the participants to have “home medical equipment” – DME.
The term “home” for the participants can be interpreted to mean –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
With certain programs and waivers, there may be a broader interpretation of what qualifies as a DME
“Consumer Direction” or “Self Direction”
On an HCBS program, or waiver, which uses “Consumer Direction” or “Self Direction” as a way of managing the funding of the project, the program beneficiaries are allotted a budget to cover their needs.
Each beneficiary is also appointed a financial advisor.
If it is apparent that the beneficiary of the program cannot do without a certain piece of equipment, and it is within their budget, they will very often be able to purchase it.
Due to the fact that the goal here is to help the individuals to remain in their homes, the items bought can go far beyond what is allowed as DME under Medicare coverage, so long as they are needed medically and within budget.
To find out more about Medicaid Self Direction, click here.
Helping the elderly return to their homes
Money follows the person – is a Medicaid based program which assists elderly adults in regaining their independence, by helping them make the transition from nursing facilities back into the community and their homes.
Assisted living is here also considered as an individual’s own home.
What may be considered a DME, is again very often different from that which is covered with Medicare, even remodeling parts of the home, if it is necessary for the participant to make the transition, is paid for by the program.
How to find the HCBS programs, waivers and 1915 waivers in your state
I have a guide with the HCBS Waivers, 1915 Waivers, HCBS Programs and the Money Follows The Person Programs for seniors which are available in each state. I have also listed all the PACE Programs – Programs of All-inclusive Care for the Elderly – for care in the home – “Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”.
How do you get DME’s with Medicaid waivers and HCBS programs ?
Step 1
– get a medical justification letter from your doctor, or therapist, which states that the equipment is medically necessary
Step 2
– find a Medicaid-approved DME supplier and give to them the medical justification letter
Step 3
– the DME supplier should fill out a Prior Approval Application for Medicaid
Step 4
– the application is then sent to the Medicaid State Office
Step 5
– if your application is unsuccessful you will be notified as to the reasons why, and given advice on how to appeal the decision
Step 6
– if approved, you will receive the DME you applied for
If your income is just too high for Medicaid
Spend Down Programs
“Spending Down” is a method used to help reduce a person’s income, or asset + income level so that they may become eligible for Medicaid.
There are two types of Spend Down –
- Asset Spend Down
- Income Spend Down
Both types involve the participant being allowed to make certain deductions from either their income, or assets, so that they may qualify for Medicaid coverage.
If you wish to find out much more about Spend Down, I have a short post here – “What is Spend Down ?”
How to find your State Medicaid State Agency
If all the technical jargon was too much for you, I would contact your state Medicaid Agency, and you can do that here.
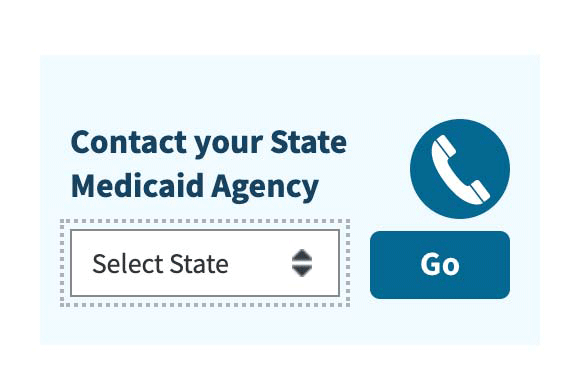
Step 1 – Once you have clicked the link to Medicaid.gov, look at the section I have outlined in the image below
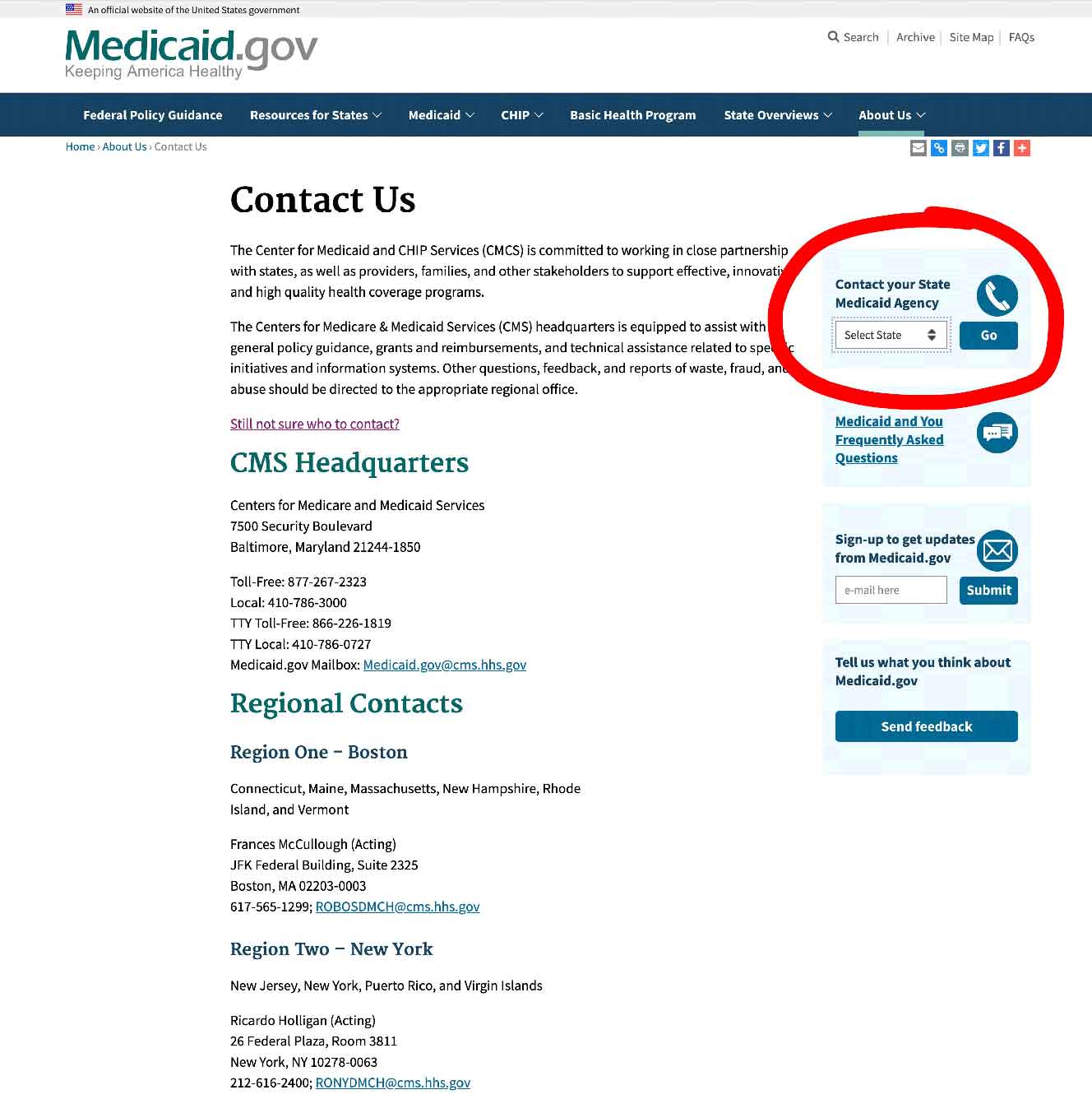
Step 2 – select your state, and click on “GO” – it will take you to your State Medicaid Agency.
State Funding Assistance
Assistive Technology Programs
Every state has Assistive Technology Programs, which serve to increase access to assistive devices in the home for those who need them – the primary focus of the programs is on the elderly and the disabled.
Assistive Technology devices can include DME, and any other equipment which makes it possible for a person to complete tasks they otherwise cannot – this can be from jar openers for arthritic hands, through to electronic digital devices.
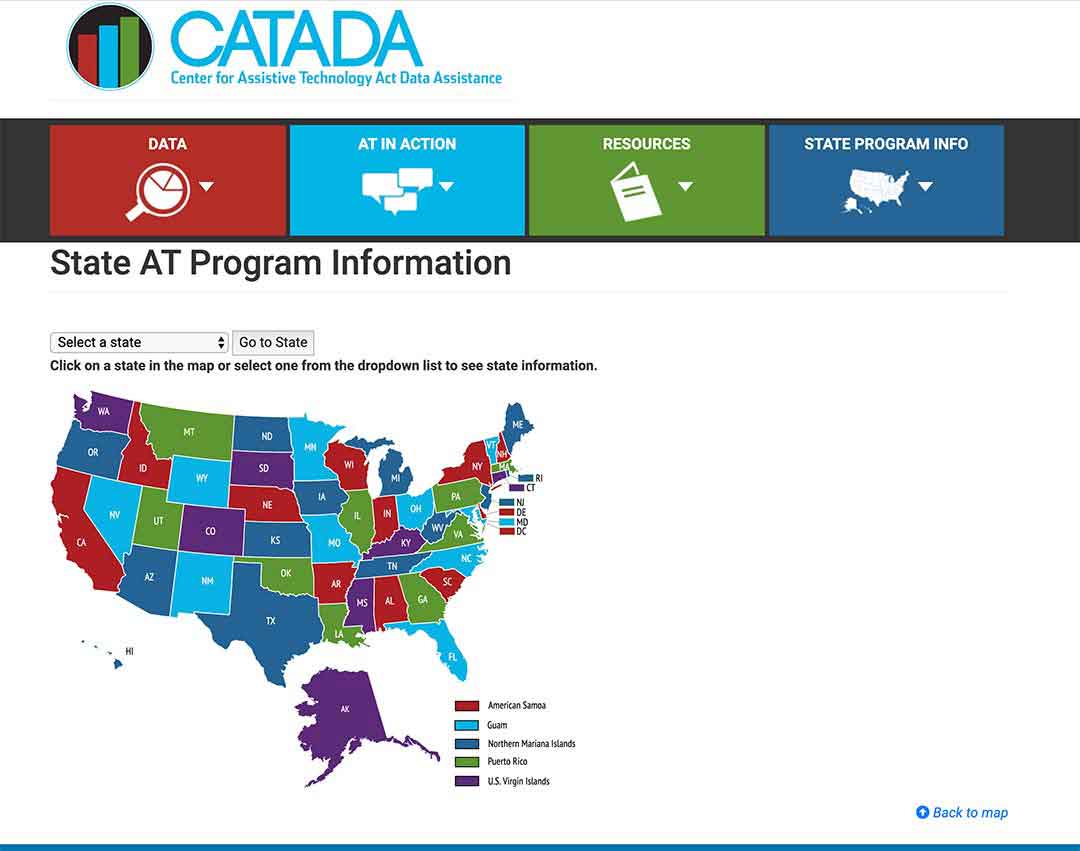
To find out what programs are in your state, click here.
Step 1/
Select your state on the map or from the drop-down menu and click on the button “Go to state”
– I chose Florida for this example.
Step 2/
Look for the link “Program Title” – for my example I outlined it in red – and click on that.
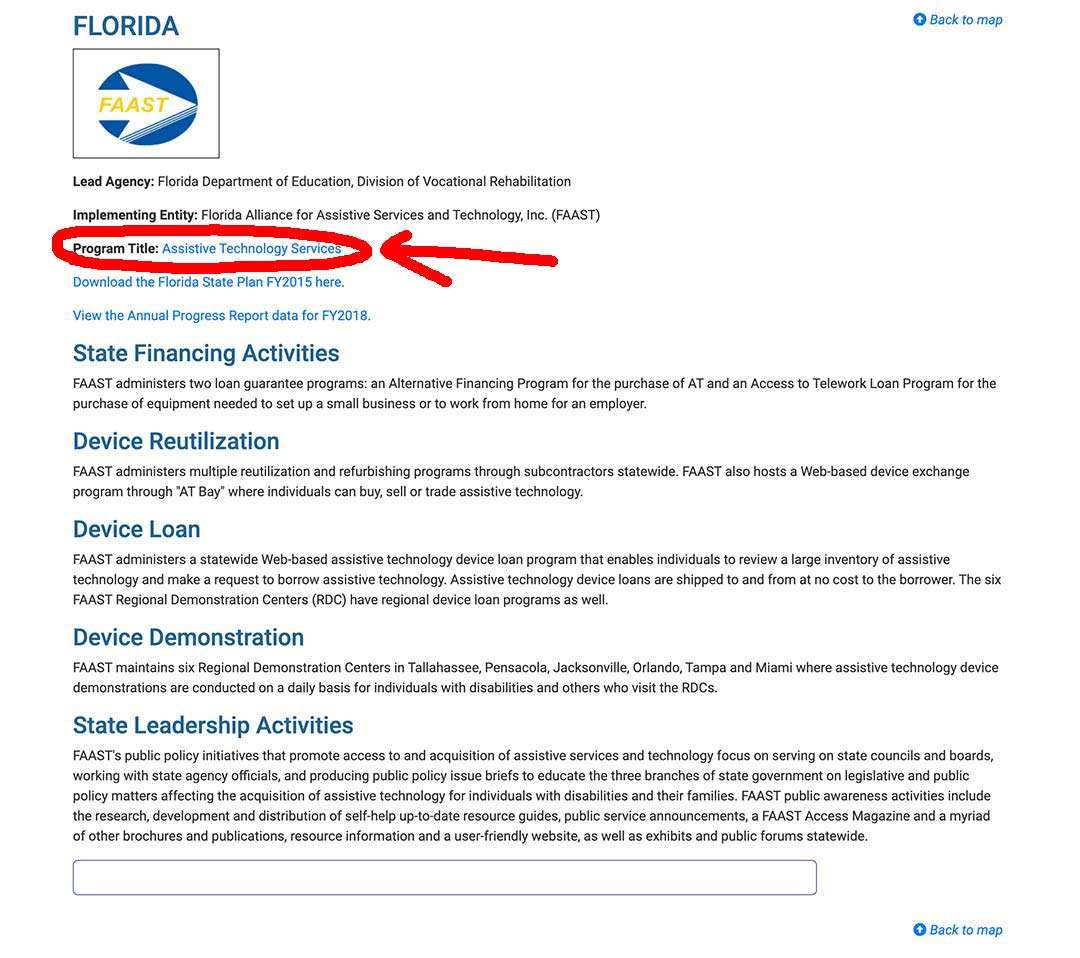
Step 3/
The State AT Program website will come up, and you can sign up, or use their contact info, to get in touch and find out what they offer to help the elderly, and if you, or a loved one, are eligible.
State Financial Assistance Programs
A number of states have non-Medicaid financial assistance programs which provide funds for the elderly to remain living in their homes.
The programs pay with grants, give loans, or will do a combination of both for participants to buy different safety items, assistive equipment, and to pay for the costs of remodeling bathrooms, wheelchair ramps, kitchen modifications – all with the aim of keeping them from unnecessarily being institutionalized.
The programs primarily focus on the elderly and the disabled.
Your local Area Agency on Aging should be able to help you locate the programs and to see if you, or a loved one, are eligible to participate.
Summary
You cannot get exercise equipment covered by Original Medicare Part B for “use in the home”, as Medicare doesn’t consider it to be “medically necessary”.
For any DME which Medicare Part B will cover, make sure you get your prescription from a Medicare-enrolled doctor, and only purchase, or rent, from a supplier if they are a Participating Supplier who accepts “assignment”.
Even if Medicare won’t cover exercise equipment, look to see if you qualify for Medicaid, a Spend-down program, or any of the other non-Medicaid state funded programs – you can always check these things with your local Area Agency on Aging.
If you have a Medicare Advantage plan, ask your provider if they cover exercise programs or gym memberships.
Good luck !
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.

