For someone who is elderly, lacking in balance and strength, getting in and out of a conventional bathtub is fraught with dangers. If you can’t afford a walk-in bathtub, one answer is to this problem is a bathtub lift. And so comes the usual question ….how to pay for it ?
Original Medicare Part B does not pay for bathtub lifts, but it does pay for patient lifts for people who confined to their bed. However, there are alternative sources of financial assistance which may help to cover the cost of a bathtub lift if you qualify.
Contents Overview & Quicklinks
Why doesn’t Medicare cover bathtub lifts ?
Does Medicare cover patient lifts ?
Does Medicare cover lift chairs ?
Does Medicare pay for bathroom equipment ?
What equipment does Medicare pay for ?
Medicare-approved supplier near me ?
List of durable medical equipment typically covered by Medicare
How can you get equipment for home use to be covered with Medicare ?
You have the signed prescription, so what’s next ?
How to avoid over-paying when you have Medicare coverage ?
How about the elderly in skilled nursing facilities ?
Do Medicare Advantage Plans cover bathtub lifts ?
Does Medicaid cover bathtub lifts ?
How to find the HCBS programs, waivers and 1915 waivers in your state ?
What is the process for obtaining items on Medicaid and state waivers, and HCBS programs ?
What if your revenue is a bit too high to qualify for Medicaid
How to get bathroom safety equipment and DME covered as a Veteran
What are bathtub lifts ?
Bathtub lifts, or bath lifts, are seats which are placed inside the bathtub.
The seat will lower the user down into the water, and raise them back up out of the water to the level of the top of the tub.
Bathtub lifts are used to help individuals who have balance, or mobility issues, to get in and out of the bathtub safely.
Bathtub lifts are not for outside the bathtub, and cannot transport a person from one location to another.
Lifts which can transport an individual from one location to another are called “patient lifts”, and are a much larger and more complex piece of equipment.
Why doesn’t Medicare cover bathtub lifts ?
Original Medicare Part B does not cover bathtub lifts, as they are considered to be a “convenience item” and “not medically necessary”.
You can check the information for yourself on the document “National Coverage Determination (NCD) for Durable Medical Equipment Reference List (280.1)” 0n the CMS. Gov (Centers for Medicare & Medicaid Services) if you click here.
Does Medicare cover patient lifts ?
Patient lifts are devices which are used to transfer a disabled individual who cannot walk from one location to another – to a chair, a wheelchair, a bedside commode or another location.
It is entirely possible to use a patient to lower an individual onto a toilet, or into a bathtub, but should not be confused with a bath lift or a toilet lift which are attached to the toilet, or placed in the bathtub, but which cannot be used to transport a disabled person from one location to another.
Seat lifts are another category of lift, and are for people who are unable to stand up without a lift, but who are able to walk with, or without, an assistive device.
Both electric and manual patient lifts are made, and even combination models.
Original Medicare Part B will typically offer 80% coverage for a manual/hydraulic full-body lift, or a stand-assist lift, “for use in the home”, so long as the lift has been prescribed by a Medicare-enrolled physician and certified as “medically necessary” as defined in the Medicare guidelines for a patient lift.
Hoyer makes a number of different types of lift, of which Medicare partially covers certain manual full-body patient lifts and the stand-assist patient lifts.
You will likely qualify for Original Medicare Part B coverage for a patient lift if you meet these Medicare criteria –
If you cannot get from your bed to a chair, a wheelchair or a commode, without the use of a lift, and would otherwise be confined to the bed.
You will likely qualify for Original Medicare Part B coverage for a multi-positional patient transfer system –
If you meet the criteria above, and also need to be transferred in a supine position, which simply means lying horizontally and facing upwards.
Does Medicare cover lift chairs ?
For Medicare, lift chairs come under the category “seat lifts”.
Only mechanical/hydraulic seat lifts may be considered for coverage by Original Medicare Part B for “use in the home”, if all the criteria are met.
Original Medicare Part B gives partial coverage to lift chairs – Medicare will typically give 80% coverage for the mechanical part of a lift chair, and only if it has been prescribed as “medically necessary” by a Medicare-enrolled physician.
Medicare’s guidelines for coverage for a seat lift mechanism in a chair lift are the following –
“Indications and Limitations of Coverage
Reimbursement may be made for the rental or purchase of a medically necessary seat lift when prescribed by a physician for a patient with severe arthritis of the hip or knee and patients with muscular dystrophy or other neuromuscular diseases when it has been determined the patient can benefit therapeutically from use of the device. In establishing medical necessity for the seat lift, the evidence must show that the item is included in the physician’s course of treatment, that it is likely to effect improvement, or arrest or retard deterioration in the patient’s condition, and the severity of the condition is such that the alternative would be bed or chair confinement.”
Source: National Coverage Determination (NCD) for Seat Lift (280.4) – which you will find here.
Original Medicare Part B does not pay for bathtub lifts, but it does pay for patient lifts for people who confined to their bed. However, there are alternative sources of financial assistance which may help to cover the cost of a bathtub lift if you qualify.
So, the coverage for a Seat Lift (the mechanism inside the lift chair) are –
- you must have severe arthritis of the hip or knee or neuromuscular disease
- you must be incapable of standing up from a standard chair with or without arms in the home
- the seat mechanism must be part of the physician’s course of treatment for you to “effect improvement, or to arrest or retard deterioration” in your condition
- once you stand, you are able to walk
Original Medicare Part B will not coverage to seat lifts mechanisms which have a spring release mechanism, which “jolt you up to a standing position”, and which do not have a recliner which will return you smoothly and gently to a seated position.
Does Medicare pay for bathroom equipment ?
Medicare Part will cover bathroom safety equipment for use in the home which it considers to be “medically necessary”, and as such, if you have Medicare part B it covers –
- walkers
- crutches
- commode chairs
each of which can help maintain balance and stability for an elderly person in the bathroom.
Unfortunately, Medicare Part B doesn’t cover items which it considers to be for comfort and not “medically necessary” such as –
- bathtub lifts
- raised toilet seats
- transfer seats
- grab bars
- shower chairs
- floor to ceiling poles
- non-slip mats
- bath chairs
If you have a Medicare Advantage Plan, or Part C as they are also known, the case may be different.
Medicare Advantage plans have to offer all the services as Original Medicare, but also has some extra benefits that they can offer, and some may offer certain bathroom equipment which is related to chronic health conditions, such as grab bars or raised toilet seats.
So, what can you do if you have Medicare Part B ?
My mom uses a walker sometimes, instead of a grab bar, to help her get in and out of the shower, as it can be re-positioned in so many ways.
If you are unable able to get in and out of the bathtub, a 3 in 1 portable commode chair is great for taking sponge baths.
After my Mom had a hip replacement, we used our portable commode chair for several weeks.
If you are strong enough, you could put a floor to ceiling pole by the bathtub, so they have something to hold onto, or get a transfer seat which is very simple to use and safe.
Although the transfer seat doesn’t lower the person into the water, they can get over the water easily to wash themselves.
I have an exhaustive article with over 50 safety tips for the bathroom that you can read here
And another long article with 30+ caregiver tips on helping an elderly parent to bathe here
What equipment does Medicare pay for ?
Medicare pays for certain durable medical equipment for use in the home when it has been prescribed as “medically necessary”.
Typical examples of the type of durable medical equipment that Medicare Part B covers for use in the home are –
- hospital beds
- wheelchairs
- bedside commodes
- walkers
- bed trapezes
Medicare does not cover equipment which is “for comfort” or “not primarily medical in nature” such as –
- raised toilet seats
- grab gars
- over bed tables
- shower chairs
For Medicare, durable medical equipment must be –
- Durable (has to endure use over a sustained period of time)
- It must be used for a medical reason, not for comfort
- Not usually useful to someone who isn’t sick or injured
- It must be used it in your home
- Able to last at least 3 years
If your equipment does not meet these basic criteria, you will likely not get coverage from Medicare Part B.
Medicare-approved supplier near me ?
To find a Medicare DME supplier in your area, use this link at Medicare.gov
If you don’t find the equipment you want on the list of Medicare covered DME’s below, you can use this link to Medicare.gov
List of durable medical equipment covered by Medicare
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
Corrective Lenses
Prosthetic Lenses
Cataract glasses (for Aphakia or absence of the lens of the eye)
Conventional glasses or contact lenses after surgery with insertion of an intraocular lens
Intraocular lenses
Important: Only standard frames are covered. Medicare will only pay for contact lenses or eyeglasses provided by a supplier enrolled in Medicare, no matter who submits the claim (you or your supplier).
How can you get equipment for home use and be covered with Medicare ?
To qualify for Medicare coverage for DME, you will need –
- to be enrolled in Medicare Part B
- a signed prescription from a Medicare enrolled doctor which qualifies the item as a medical necessity
- purchase the DME’s through a Medicare-enrolled supplier
If you are claiming for coverage for DME for use in your “home”, a hospital, or nursing home, does not qualify as a “home” for Medicare part B, however you are covered under Medicare Part A.
A long term care facility in the community, such as an assisted living facility, does qualify for medicare Part B.
What is a home for Medicare Part B ?
The following are considered a “home” for Medicare –
- your home
- the family home
- living in the community, such as assisted living
You have the prescription, so what’s next ?
Once Medicare agrees to cover your purchase, you will still have to pay your co-payment of 20% of the Medicare-approved price of the item and your annual deductible (if it hasn’t already been met). Medicare pays the remaining 80% of the Medicare-approved price.
Medicare will either purchase or pay a rental for your item.
With cheaper items Medicare tends to purchase these, but for more expensive items such as hospital beds for example, Medicare pay a monthly rental for the equipment.
If the item is rented by Medicare from a Medicare-approved supplier who is accepting assignment, you will pay a monthly co-payment of 20% of the Medicare-approved rental price, and Medicare will pay the remaining 80%.
How to avoid over-paying when you have Medicare coverage ?
So that you pay the least amount possible, you must make sure that you are using a Medicare-enrolled “participating” supplier who accepts “assignment”. This ensures that you are only going to pay their Medicare co-pay of 20% of the Medicare-approved price, and if you haven’t already met it, your annual Medicare Part B deductible.
This is why –
There are two categories of Medicare-enrolled suppliers –
- Medicare Suppliers
- Medicare “Participating” Suppliers
The difference between the two categories is that –
Medicare “Participating” Suppliers have agreed to accept what is called “assignment” – this restricts the supplier to only charging the Medicare-approved price for any Durable medical Equipment.
This means that when you buy your DME from a Medicare-enrolled “participating” supplier, you will be paying the least possible amount – 20% of the lowest possible price, plus your annual deductible if you haven’t yet met that.
What happens when your parent is not buying from a Participating Supplier ?
A supplier who is Medicare enrolled, but not a “Participating” Supplier, accepts to take payment from Medicare, but isn’t obliged to accept “assignment”. As a result, they are then free to charge as 15% more for the item, which can be considerably higher than the Medicare-approved price, and this excess is passed on to the buyer. Do note that certain states have laws which won’t let the suppliers go as high as 15% extra.
How about the elderly in skilled nursing facilities ?
If your loved one, is in a skilled nursing facility or hospital, they will be covered by Medicare Part A. Medicare requires that the nursing facility provide all medically necessary equipment for 100 days.
Do Medicare Advantage plans cover bathtub lifts ?
For Medicare Advantage Plans, otherwise known as Medicare Part C, your loved ones will need to check with their plan provider to find out which DME’s are covered.
These plans are run by private Medicare-approved companies contracted by Original Medicare to provide at least the same Medicare services as Original Medicare Parts A and B.
Legally, beneficiaries of Medicare Advantage Plans are entitled, at a minimum, to the same DME’s as Original Medicare, but they may also have, along with vision and hearing aids, some new benefits as of 2020.
In 2019 the Centers for Medicare & Medicaid announced an expansion of the coverage of Medicare Advantage and Part D –
Beginning in 2019, Medicare Advantage plans can now offer supplemental benefits that are not covered under Medicare Parts A or B, if they diagnose, compensate for physical impairments, diminish the impact of injuries or health conditions, and/or reduce avoidable emergency room utilization.
The text source – “CMS finalizes Medicare Advantage and Part D payment and policy updates to maximize competition and coverage” April 1, 2019. You can read the text here.
It is this expansion which will see the addition of some benefits which are for chronic conditions, and among these will be certain items of bathroom safety for individuals with mobility conditions.
You will need to scour the plans on offer to find one with bathroom equipment, and always remember to stick within the provider’s network.
Free assistance with Medicare
SHIP – State Health Insurance Assistance Programs –
You can get free guidance about Medicare, Medicaid and Medigap from your state program.
I have a short article explaining how to find your local SHIP, and you can find that here – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
Does Medicaid cover bathtub lifts ?
The structure for Medicaid funding for programs is both federal and state funding based. There are hundreds of Medicaid programs and waivers across the different states, and they can vary quite widely, as each state can make it own funding decisions.
Medicaid programs are for people with extremely low incomes; mainly the elderly and the disabled, but also low income families.
Medicaid will pay for “home medical equipment”, and will very often cover 100% of the cost.
When Medicaid uses the term “home” it means the person must be in –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
The following Medicaid and state programs are designed to help people stay residing in their homes and to provide the support they need.
The Medicaid programs for the home are called Home and Community Based Services (HCBS), Waivers, or 1915 Waivers.
Programs can vary widely from state to state, but most do allow for a good range of DME’s, and some are broader in their range than Medicare.
Consumer Direction – The beneficiaries of some waivers are allotted budgets, and with the help of financial planners, they use the budgets to cover their requirements. The money can be used to buy durable medical equipment which is necessary for the beneficiaries to stay living in their homes.
Money follows the person – these programs are designed to assist people in leaving nursing facilities to return to their own homes, or assisted living facilities. The programs will pay for equipment which is necessary to the people being able to live in their homes.
How to find HCBS programs, waivers and 1915 waivers and their eligibility criteria in your state
I have an article where you can find all the HCBS Waivers, 1915 Waivers, HCBS Programs and the Money Follows The Person Programs for seniors which are available in each state, along with links to the different program websites. Also listed are all the PACE programs which are for All-inclusive care in the home –“Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State.
What is the process for obtaining items on Medicaid and state waivers, and HCBS programs ?
Step 1
– the doctor, or therapist, has to provide a medical justification letter, stating it is medically necessary
Step 2
– find a Medicaid-approved DME supplier, and give them the medical justification letter
Step 3
– the Medicaid-approved supplier fills out a Prior Approval Application form for Medicaid
Step 4
– the Prior Approval Application is sent to the Medicaid State Office
Step 5
– if you are unsuccessful you will be contacted and given the reasons as to why, as well as advice on how to make an appeal
Step 6
– if approved, you will receive the DME.
What if your revenue is too high to qualify for Medicaid ?
The Spend Down Program
Spend-Down programs are designed to help reduce a person’s income, or income + asset level so that they may become eligible for Medicaid, HCBS’s and waivers.
The simplest method employed to achieve this, “Income Spend Down”, is to subtract a person’s medical expenses from their income, and should the result be that their income level falls below the Medicaid eligibility limit, the person will then qualify for Medicaid.
The second method “Asset Spend Down” is quite a lot more complex, and involves, as the title indicates, the person’s assets.
If you want to learn more, I have an article where I explain who can qualify for Spend Down, the expenses they can deduct and how you know if you qualify. You will find that here – “What is Spend Down ?”
To find your State Medicaid State Agency
If you want to discuss things, or to email someone, you can contact your state Medicaid Agency here.
Step 1 –
Click the link to Medicaid.gov and look for the section that I have outlined in red.
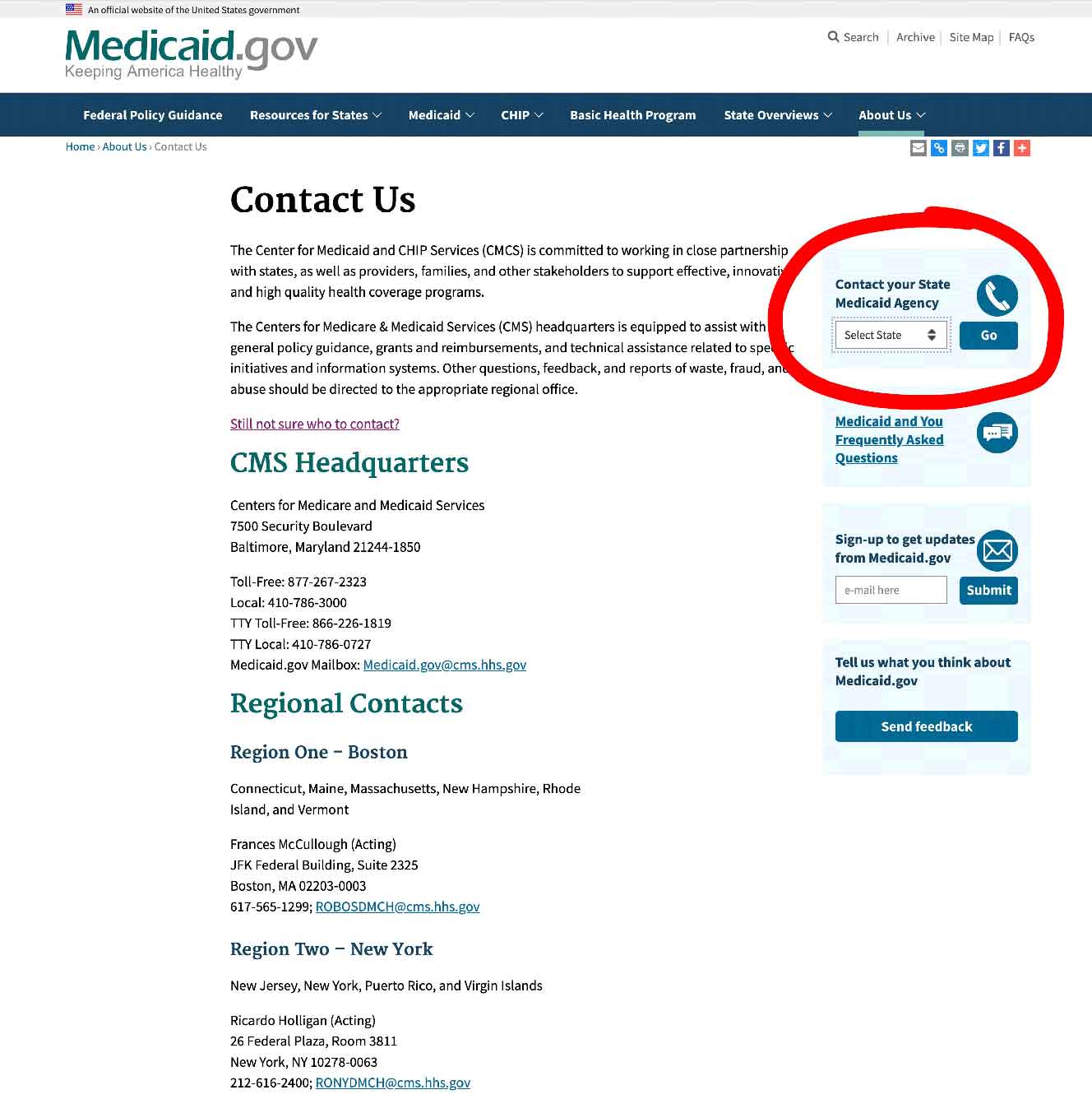
Step 2 –
Select your state and click on the button they have marked “GO” – it will take you to your State Medicaid Agency with all their contact info.
State Funding Assistance
Assistive Technology Programs
A grant – The Assistive Technology Grant – is given to each state in the US, by the government, to help increase access to assistive technologies in the home. The primary groups they are trying to reach are the disabled and the elderly.
The term “assistive technologies” refers to all kinds of equipment which make it possible for a person to achieve an action that they cannot otherwise achieve. It can be a special type of tin opener, or a wheelchair.
Each state must use the grant to set up their own “State Assistive Technology Program“.
State Assistive Technology Programs generally have at least these services –
- an online equipment exchange on which all state residents can post used assistive devices and medical equipment for sale, donation, or exchange
- a main website which lists all the program’s services, and which answers inquiries about such things as eligibility
- reuse and refurbishment centers which are run by the state program, and often community partners, to provide extremely low cost or free “gently used” equipment for the disabled and the elderly
- loan closets as part of their programs are quite common, and these can be either long or short term
Assistive Technology Programs will register state residents who need and are eligible for help, and will contact them when specific equipment or services become available.
Your State Assistive Technology Program website will have all the necessary information, so start any inquiries there.
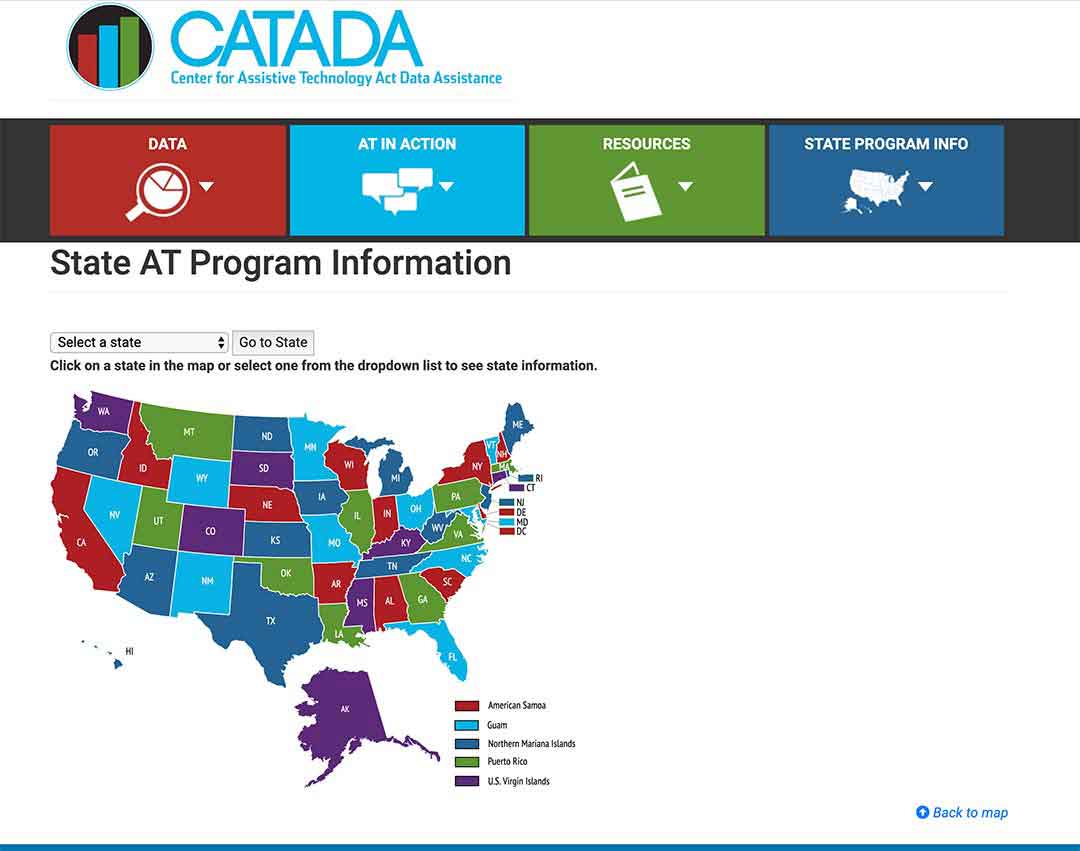
To see what projects are in your state, click here.
Follow the steps below to see the projects in your state
Step 1/
Pick your state on the map or the drop-down menu, and click on “Go to state”
– I chose Florida for this example.
Step 2/
Click on the link “Program Title” – for my example, I outlined it in red.
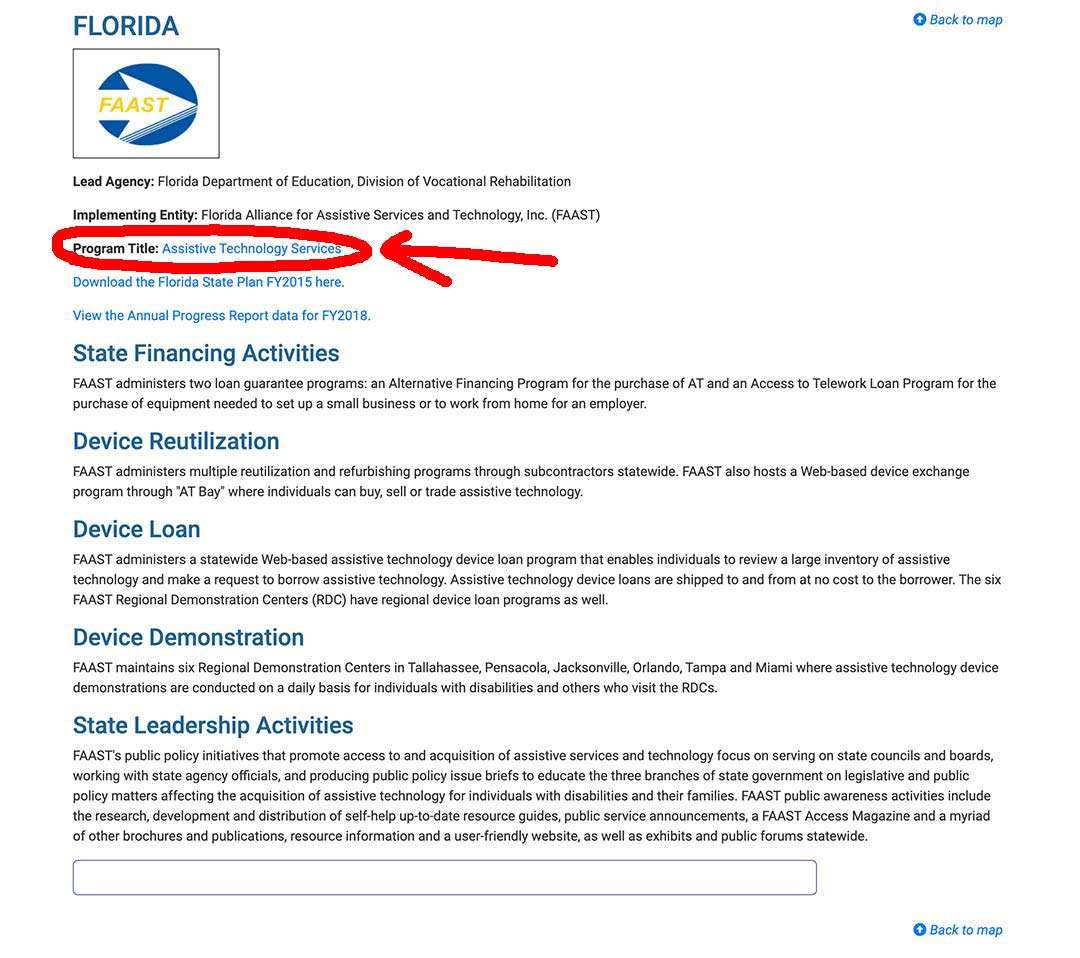
Step 3/
The AT Program state website will come up, and you can register, or use their contact info.
State Financial Assistance Programs
State Financial Assistance Programs are non-Medicaid programs designed to help the elderly to remain living in their own homes, and will pay for assistive devices, safety equipment, durable medical equipment, as well as home modifications.
To achieve these goals, the programs will pay for what is required with grants or loans, or sometimes a combination of the two.
Go speak with your local Area Agency on Aging to get advice on these programs for the elderly, and find out if there is one in your state.
How to get bathroom safety equipment and DME’s covered as a Veteran
For veterans, the Department of Veterans’ Affairs has different grants, programs and forms of financial assistance which will help cover the cost of items needed in the home.
Veterans are beneficiaries of healthcare under the VA Medical Benefits Package.
For veterans, the law provides that the VA has to give eligible veterans hospital care and outpatient care services, which they call “needed.” The VA defines “needed” as “a care, or a service, which promotes, preserves or restores health”.
You can find out about local VA Medical Centers and other offices in each state here.
These are just some different forms of assistance for you to look at if your parent is a veteran.
- Tricare for life
- Tricare
- Veterans Directed Home and Community Based Services
- ChampVA for Life
Summary
You can’t get bathtub lifts covered by Medicare parts A and B, or for that matter most other bathroom safety equipment devices for the elderly.
There are, though, possibilities of getting bath lifts with the different Medicaid state programs, non-medicaid state programs for the elderly, or if you are a veteran, certain programs may be able to cover the equipment you need through the VA medical Benefits Package.
Don’t forget that bathtub lifts are not to be confused with patient lifts, which are partially covered if you meet the Original Medicare Pat B criteria.
A patient lift can be used to lift and place an individual in a bathtub, but these are not electric lifts which are placed in the shower and rise up and down. Patient lifts are large lifts which are covered for patients who are bed bound, and otherwise cannot be moved without a number of caregivers.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.

