As our loved ones get older and their health declines, even if it is not serious, the costs of all the different pieces of equipment they need starts to really add up, and you really have to brace yourself for what is coming next … Please excuse me that little pun, but I couldn’t resist. And I hope that you don’t need one for your elderly parent, or loved one, but today’s topic is neck braces.
Does Medicare cover neck braces ? Yes, Medicare Part B typically covers 80% of the Medicare-approved price of neck braces prescribed as “medically necessary” by a Medicare-enrolled doctor, and which are bought, or rented, from a Medicare-approved supplier.
Contents Overview & Quicklinks
Medicare qualifying guidelines for neck braces
Medicare-approved neck braces ?
Does Medicare cover back braces ?
Medicare qualifying guidelines for back braces
Medicare-approved back braces ?
How much is a back brace with Medicare ?
Decompression back braces covered by Medicare
Does Medicare cover knee braces ?
Medicare knee brace qualifying guidelines
Medicare-approved knee braces ?
Medicare-approved braces and devices
Does Medicare cover bathroom equipment ?
Medicare 5 year replacement rule
What equipment does Medicare cover ?
How do you get coverage from Medicare Part B for DME ?
Okay, you have your signed prescription, what’s next ?
Medicare-enrolled Supplier near me ?
Are neck braces covered by Medicare Advantage plans ?
List of Durable Medical Equipment typically covered by Medicare
Free help with understanding Medicare
Does Medicaid cover neck and other braces ?
Programs and waivers which most likely cover DME for “in home use” ?
How to find the HCBS programs, waivers and 1915 waivers in your state ?
How to get DME with Medicaid, state waivers and HCBS programs ?
If your income is a bit too high to qualify for Medicaid
Medicare qualifying guidelines for neck braces ?
Neck braces, or cervical orthoses, are covered under the Durable Medical Equipment Orthotics Benefit.
Medicare part B will cover a neck brace if it is “medically necessary” under the Benefit for Orthotics or Braces.
To qualify for a neck brace, you must need one of the following–
- stabilization of the neck because of a weakness or deformity
- restriction of the movement of the neck due to an injury or disease
- limitation of movement of the neck during recovery from a surgical procedure
You will need to have a face-to-face appointment with a Medicare-enrolled doctor and to get a signed prescription which certifies that you qualify under one of the above criteria, and as such that a neck brace is “medically necessary”.
Medicare-approved neck braces ?
You are allowed to choose from, either Custom Fitted, or Off-The-Shelf neck braces with coverage under Medicare part B.
The difference between the two types of braces –
Custom Fitted Braces –
Even though custom fitted braces may come in kit form, they require fitting by a certified Orthotist, as they may demand an important amount of modification during the fitting process to make a proper fit.
Off-The-Shelf braces –
Off-The-Shelf braces may come as a kit and will require some assembly, but this should only be minimal adjustments, which the beneficiary can easily do themselves.
They should not require the help of a certified Orthotist for the best possible fit.
The passage below is from the Medicare Benefits Policy Manual Chapter 15 – Revised 2019 which you can find here.
130 – Leg, Arm, Back, and Neck Braces, Trusses, and Artificial Legs, Arms, and Eyes (Rev. 1, 10-01-03) B3-2133, A3-3110.5, HO-228.5, AB-01-06 dated 1/18/01
“These appliances are covered under Part B when furnished incident to physicians’ services or on a physician’s order.
A brace includes rigid and semi-rigid devices which are used for the purpose of supporting a weak or deformed body member or restricting or eliminating motion in a diseased or injured part of the body. Elastic stockings, garter belts, and similar devices do not come within the scope of the definition of a brace.
Adjustments, repairs and replacements are covered even when the item had been in use before the user enrolled in Part B of the program so long as the device continues to be medically required.”
Does Medicare cover back braces ?
To get coverage for a back brace under Medicare Part B, you will again need to get a signed prescription from a Medicare-enrolled doctor, certifying that the back brace is “medically necessary” for you.
You must have a face-to-face appointment with the doctor so that he can make a proper diagnosis, and it must be held within the prior six months to the date the claim is made.
Medicare qualifying guidelines for back braces
To get coverage for a back brace, as I have already said, you will first need to obtain a signed prescription from a Medicare-enrolled doctor, stating that a back brace is “medically necessary”.
Medicare has guidelines about when coverage may be given to a patient for a back brace.
The following text is from Medicare’s guidelines for back braces, which they are calling “Spinal Orthosis” –
“A spinal orthosis (L0450 – L0651) is covered when it is ordered for one of the following indications:
1. To reduce pain by restricting mobility of the trunk; or
2. To facilitate healing following an injury to the spine or related soft tissues; or
3. To facilitate healing following a surgical procedure on the spine or related soft tissue; or
4. To otherwise support weak spinal muscles and/or a deformed spine.
If a spinal orthosis is provided and the coverage criteria are not met, the item will be denied as not medically necessary.”
In short, if you are to get coverage, the back brace has to be used to do one of the following –
- to reduce pain by restricting movement of the torso
- promote with the healing of the spine or muscles, ligaments after an injury, or after surgery
- give support to a weak spinal muscle and/or a deformed spine
Medicare-approved back braces ?
Medicare will only cover rigid or semi-rigid braces of any type.
The two following exerts were taken from the Medicare Benefit Policy Manual, Chapter 15 –
“A brace includes rigid and semi-rigid devices which are used for the purpose of supporting a weak or deformed body member or restricting or eliminating motion in a diseased or injured part of the body.”
The text goes on to say –
“Back braces include, but are not limited to, special corsets, e.g., sacroiliac, sacrolumbar, dorsolumbar corsets, and belts.”
Below are some of the more well-known brands –
- Aspen
- Corflex
- Comfortland
- Ossur
Your Medicare-enrolled supplier will have the brands he works with, so if you don’t find the brand you want, you may have to seek out a number of Medicare-enrolled suppliers.
How much is a back brace with Medicare ?
If you are enrolled in Medicare Part B and you have had a back brace prescribed as “medically necessary” by a Medicare-enrolled physician, and you purchase your back brace from a Medicare-approved “Partcipating” Supplier, Medicare will pay 80% of the price of the back brace for you.
You will have to pay your 20% co-insurance, and your deductible if it applies.
If you use a Medicare-approved supplier, but who is not a “Paticipating” supplier, you may have to pay up to 15% more.
If you do not use a Medicare-approved physician, or a Medicare approved supplier, or both, you will have to pay for everything.
Decompression back braces covered by Medicare
Medicare Part B will, under certain conditions, cover some decompression back braces.
Here are two examples of decompression back braces covered by Medicare are –
- Dr Ho’s decompression back belt
- DDS 500 Lumbar decompression brace
Does Medicare cover knee braces ?
Medicare Part B will typically give coverage to knee braces, just so long as you have a prescription from a Medicare-enrolled doctor certifying it is “medically necessary”.
Medicare knee brace qualifying guidelines
Medicare Part B gives covers knee braces as Durable Medical Equipment under the Orthotics Benefit.
To qualify for a knee brace, you must first have an in-person appointment with a Medicare-enrolled doctor, so that they can make a diagnosis.
The doctor is going to have to find that a knee brace is “medically necessary” in your case, in accordance with the Medicare guidelines.
Medicare considers a knee brace to be “medically necessary” when –
- a person is able to walk
- a knee requires stabilization because of weakness or deformity
- you have had a recent injury to the knee
- you recently had a knee surgery, such as a knee joint replacement
If you qualify, your Medicare-enrolled doctor will give you a prescription certifying that your knee brace is “medically necessary”.
The doctor will prescribe a certain type of knee brace for your condition, with a specific equipment code, and that is the only type of brace you will be allowed to have.
The following text from Medicare outlines the functions the braces must be able to perform, and that they may be either rigid, or semi-rigid.
Medicare Benefits Policy Manual Chapter 15 – Revised 2019 here
130 – Leg, Arm, Back, and Neck Braces, Trusses, and Artificial Legs, Arms, and Eyes (Rev. 1, 10-01-03) B3-2133, A3-3110.5, HO-228.5, AB-01-06 dated 1/18/01
These appliances are covered under Part B when furnished incident to physicians’ services or on a physician’s order.
A brace includes rigid and semi-rigid devices which are used for the purpose of supporting a weak or deformed body member or restricting or eliminating motion in a diseased or injured part of the body. Elastic stockings, garter belts, and similar devices do not come within the scope of the definition of a brace.
Adjustments, repairs and replacements are covered even when the item had been in use before the user enrolled in Part B of the program so long as the device continues to be medically required.
Medicare-approved knee braces ?
Medicare approves four types of knee braces
Medicare coverage includes four types of knee orthotics.
Devices must help manage stability or give pain relief and allow the patient to carry out daily functions.
Functional – these braces are worn to give support to knees which have been injured in the past.
Functional braces may be used after surgeries to give support to the knee.
Rehabilitative or Postoperative – these braces, while allowing the joint to move, will protect ligaments and tendons after surgery by limiting potentially harmful movements during the rehabilitation.
Unloader or Off-loader – often to reduce pain from osteoarthritis.
Unloader braces take pressure off the sides of the knee by limiting the sideways movement, and by putting the pressure on the thigh.
Prophylactic – made for the prevention of knee ligament injuries, in particular the MCL ligament, these are frequently used by athletes and footballers.
Custom Fitted and Off-The-Shelf
Medicare Part B allows both Custom Fitted and Off-the-Shelf knee braces.
Custom Fitted braces –
Custom fitted braces can require a significant amount of alteration during the fitting to make them fit correctly, this has to be done by a certified Orthotist.
Off-The-Shelf braces –
These may be supplied as a kit, requiring only a minimal adjustment for to be fitted properly.
These should not require the help of a certified Orthotist for the best possible fit.
Medicare-approved braces and devices
The following kinds of braces are covered by Medicare Part B, under certain circumstances –
Back braces –
- Lumbar Sacral Braces
- Thoracic Lumbar Sacral Braces
Shoulder braces
- shoulder immobilizers
- shoulder cradles
- shoulder stabilizers
Neck braces
- cervical collars
- some cervical traction collars
Foot and ankle braces –
- ankle-foot (AFO)
- knee-ankle-foot (KAFO)
Knee braces –
- rehabilitative
- functional
- unloader or off-loader
- prophylactic
Elbow braces –
- elbow immobilizer
Wrist braces –
- braces
- supports
- splints
Does Medicare cover bathroom equipment ?
Medicare Part B will only cover durable medical equipment for use in the home, and that which it considers to be “medically necessary”.
As a result, a lot of safety equipment which you may have thought Original Medicare Part B would cover for use in the home, is not covered.
The majority of the equipment used in bathroom for safety is not covered, such as –
- grab bars
- raised toilet seats
- bath lifts
- bath seats
- floor to ceiling poles
- shower chairs
- bath chairs
- transfer seats
- toilet safety frames
Most of the items aren’t covered because they are “not medical in nature” or they are “for comfort”.
Original Medicare does though consider medical equipment for those mobility issues as “medically necessary”, and if you have difficulty walking, or standing, you may qualify for coverage of the following items –
- crutches
- walkers
- bedside commodes
There are some items which are a little more difficult to understand, for example if you are bed bound, a patient lift, as it is called by Original Medicare, is covered, so that you may get into a wheelchair etc.
But if you cannot get into the bathtub, but you can get out of bed, you may not get a bath lift.
The lift to help you out of bed is considered “medically necessary”, so that you are not left stuck in bed, and the bath lift is considered a comfort item which Medicare Part B will not cover.
Patient lifts will though transport and place someone in a bathtub who cannot walk.
Luckily for some, Medicare Advantage Plans are different from Original Medicare, in that they are now starting to be allowed to offer more benefits.
Medicare Advantage Plans are now being permitted to offer plans with benefits for individuals with chronic illnesses, and some of these benefits include, or will soon include, bathroom safety equipment for certain illnesses.
Medicare 5 year replacement rule
DME can be replaced by Medicare part B when they are –
- worn out from use
- that have been in your possession throughout their lifetime
- too far gone to be fixed
Two final points –
- the shortest period to be considered a lifetime for DME is five years
- the lifetime may vary depending on the type of equipment
Typically, a neck brace which is “worn out” may be replaced every five years, if it has been in the beneficiary’s possession for that whole period.
Knee braces though have a lifetime of 1 1/2 to 2 years.
Medicare Part B will pay to repair non-functioning DME which haven’t reached the end of their lifetime, but will not pay more than the cost of an equivalent replacement.
If you are replacing an item, you have to go through the whole Medicare claim procedure with the doctor and supplier all over again.
What equipment does Medicare cover ?
The equipment that Medicare covers for use in the home is called “durable medical equipment”, or DME.
The equipment is durable, as opposed to being disposable.
Medicare does not cover disposable equipment, or supplies.
Durable medical equipment must –
- tolerate constant use over a sustained period of time – durable
- be primarily medical in nature – not for comfort
- be useful only to a person who is ill
- be principally for use in the home
- have a minimum lifetime of at least 3 years
How do you get coverage from Medicare Part B for DME ?
For you to get covered by Medicare Part B for your durable medical equipment for “use in the home” –
- you are going to have to be enrolled in Medicare Part B
- you must have a Medicare-enrolled doctor to give you a signed prescription which certifies that the equipment is a medical necessity
- the equipment must come through a Medicare-enrolled supplier
Medicare defines “living at home” as –
- living in your own home
- living in the family home
- living in the community, such as assisted living
Okay, you have your prescription, what’s next ?
It’s time to choose your DME.
Your doctor will doubtless be able to advise you on some of this –
- you need to locate a Medicare-enrolled supplier who has your type of DME
- you only want to deal with a supplier who is a Medicare-enrolled “participating supplier who accepts “assignment” – doing this you will have the lowest possible costs
- the models of DME Medicare covers are rather basic, although if you are willing to pay, you may sometimes be able to upgrade to a model you prefer
- make your choice from what is available
- fill out any compulsory paperwork for Medicare with the supplier
Medicare part B covers 80% of the Medicare-approved price for DME if you used a Medicare-enrolled supplier with a signed prescription from a Medicare-enrolled doctor saying that your item is “medically necessary”.
If you used a Medicare-enrolled “participating” supplier who accepts “assignment”, you will just have to pay your Medicare 20% co-payment of the Medicare-approved price for your DME, and your deductible if it applies.
Remember to always go through a Medicare-enrolled supplier who is a Medicare-enrolled “Participating” supplier who accepts “assignment”, so that you don’t end up paying money that you shouldn’t have to.
Medicare both rents and purchases DME – If your equipment is rented by Medicare from the supplier, you will just pay a 20% co-payment of the monthly rental each month, and at the outset, if it applies, your deductible.
Medicare-enrolled DME Supplier near me
You can use this link to find a Medicare-enrolled supplier who is local to you – Medicare.gov
Are neck braces covered by Medicare Advantage plans ?
Medicare Advantage plans will, by law, cover, at the least, everything covered by Medicare Parts A and B, and sometimes, depending on the plan, some extras.
So, yes, neck braces are covered by Medicare Advantage plans, and the same Medicare guidelines for use in the home apply as for Medicare Part B.
You will need to contact your plan provider and find out which doctors and suppliers to use, if you don’t already know.
Don’t go outside your provider’s network, as you will doubtless lose coverage and have to pay for the brace yourself.
List of durable medical equipment covered by Medicare
If you don’t find the equipment you are looking for in my list of Medicare covered DME below, go to this link to Medicare.gov
Air-Fluidized Bed
Alternating Pressure Pads and Mattresses
Audible/visible Signal Pacemaker Monitor
Pressure reducing beds, mattresses, and mattress overlays used to prevent bed sores
Bead Bed
Bed Side Rails
Bed Trapeze – covered if your loved one is confined to their bed and needs one to change position
Blood sugar monitors
Blood sugar (glucose) test strips
Canes (however, white canes for the blind aren’t covered)
Commode chairs
Continuous passive motion (CPM) machines
Continuous Positive Pressure Airway Devices, Accessories and Therapy
Crutches
Cushion Lift Power Seat
Defibrillators
Diabetic Strips
Digital Electronic Pacemaker
Electric Hospital beds
Gel Flotation Pads and Mattresses
Glucose Control Solutions
Heat Lamps
Hospital beds
Hydraulic Lift
Infusion pumps and supplies (when necessary to administer certain drugs)
IPPB Machines
Iron Lung
Lymphedema Pumps
Manual wheelchairs and power mobility devices (power wheelchairs or scooters needed for use inside the home)
Mattress
Medical Oxygen
Mobile Geriatric Chair
Motorized Wheelchairs
Muscle Stimulators
Nebulizers and some nebulizer medications (if reasonable and necessary)
Oxygen equipment and accessories
Patient lifts (a medical device used to lift you from a bed or wheelchair)
Oxygen Tents
Patient Lifts
Percussors
Postural Drainage Boards
Quad-Canes
Respirators
Rolling Chairs
Safety Roller
Seat Lift
Self-Contained Pacemaker Monitor
Sleep apnea and Continuous Positive Airway Pressure (CPAP) devices and accessories
Sitz Bath
Steam Packs
Suction pumps
Traction equipment
Ultraviolet Cabinet
Urinals (autoclavable hospital type)
Vaporizers
Ventilators
Walkers
Whirlpool Bath Equipment – if your loved one is home bound and the pool is medically needed. If your loved one isn’t home bound, Medicare will cover the cost of treatments in a hospital.
Prosthetic and Orthotic Items
Orthopedic shoes only when they’re a necessary part of a leg brace
Arm, leg, back, and neck braces (orthotics), as long as you go to a supplier that’s enrolled in Medicare
Artificial limbs and eyes
Breast prostheses (including a surgical bra) after a mastectomy
Ostomy bags and certain related supplies
Urological supplies
Therapeutic shoes or inserts for people with diabetes who have severe diabetic foot disease.
Free help with understanding Medicare
SHIP – State Health Insurance Assistance Programs –
Free counseling services about Medicare, Medicaid and Medigap are offered over the phone (mostly) by all state programs – SHIPs.
Here is a short guide outlining how to find your SHIP – “Free Help Understanding Medicare And Medicaid ? Here’s Where You Get It”.
It is as easy as giving them a call.
Does Medicaid cover neck braces ?
Medicaid has a very different funding structure from Medicare, as its programs gain funding both federally and by each individual state.
Concretely, this results in each individual state having quite a lot of wiggle room in what it does with its Medicaid programs, just so long as it keeps within the main Medicaid guidelines.
It is normal for Medicaid to permit a state to waive some of its eligibility requirements for certain programs, so that they may be able to give health care to a group of people who might otherwise not receive any.
This permission to ignore some normal eligibility requirements is known as a Waiver, and each waiver can have very specific eligibility requirements of its own, targeting specific groups of the population, and often with a limited number of places.
There are hundreds of such waivers, all with different eligibility across the US.
Care for the elderly in the home – Medicaid and state programs
Programs providing care within the home, and which are principally for the elderly, very low income families and the disabled are called “Home and Community Based Services” (HCBS), “Waivers” or “1915 Waivers”.
HCBS programs, waivers, and 1915 waivers exist to help the participants to maintain their independence, and will all help to pay for “home medical equipment”, very often covering the whole cost.
See if you are eligible for an HCBS program or waiver, by contacting your State Medicaid Agency here.
You can also find out more at your local Area Agencies on Aging.
Use the link below to find out more on HCBS programs or waivers –
https://www.medicaid.gov/medicaid/hcbs/authorities/index.html
A “home” for Medicaid is any of the following –
- their own home
- their family home
- a group home
- an assisted living facility
- a custodial care facility
Programs and waivers which most likely cover more a wider range DME for “in home use”
HCBS programs and waivers working with “Consumer Direction”or “Self Direction”
“Consumer Direction”or “Self Direction” is essentially a self-managed program model, where the participant makes a lot of the decisions about how their program budget is spent.
To help guide them, they will be appointed a financial advisor.
So long as the participant’s budget has enough money in it, equipment essential to them participating in the program, or waiver, is covered.
Learn more about Medicaid Self Direction here.
Money Follows the Person
This is a federal Medicaid program which was set up help elderly adults living in nursing homes to move back into their own homes.
The Medicaid program assists the states with funding to set up Money Follows The Person Programs.
The states can use HCBS waivers which already exist, or they can establish whole new programs, to help the elderly to make the transition back to their homes.
The programs will give the money required for making the transition, and for the elderly persons to maintain their independence. This can be buying standard DME or remodeling parts of a home.
How to find the HCBS programs, waivers and 1915 waivers in your state
I have written up a guide with all the Medicaid HCBS waivers and programs for seniors in each US state, as well as any Money Follows The Person Programs and PACE Programs (Programs of All-inclusive Care for the Elderly).
Just go to your state in the list, and you will find a list of what is offered with the links to the appropriate websites which run the programs.
The guide is here – “Medicaid Home and Community Based Services Waivers and Programs For Seniors Listed By State”.
How to get DME with Medicaid, state waivers and HCBS programs ?
Step 1
– the doctor, or therapist, has to provide a medical justification letter, stating it is medically necessary
Step 2
– find a Medicaid-approved DME supplier, and give them the medical justification letter
Step 3
– the Medicaid-approved supplier fills out a Prior Approval Application form for Medicaid
Step 4
– the Prior Approval Application is sent to the Medicaid State Office
Step 5
– if you are unsuccessful you will be contacted and given the reasons as to why, as well as advice on how to make an appeal
Step 6
– if approved, you will receive the DME
If your income is a bit too high to qualify for Medicaid
Spend Down Programs
Spend Down programs are a Medicaid initiative which gives more people access to Medicaid coverage by reducing a program participant’s income level, or income level + asset level, through the deduction of certain expenses, loans and debt payments.
There are two methods –
- Income Spend Down
- Asset Spend Down
Income Spend Down is the easier of the two methods (meaning easier to understand and also put into practice), and basically allows a participant to deduct certain medical expenses from their income so that their income falls below the Medicaid limit.
Asset Spend Down is quite a lot more complicated, as it involves getting shot of certain assets so that the person doesn’t have too many assets to qualify for Medicaid. You can deduct, amongst other things, loan and debt repayments.
Here is an article about how it works and eligibility for Spend Down Programs, – What is Spend Down ?
To find your State Medicaid State Agency
If you just want to talk to, or to email someone, contact your state Medicaid Agency here
Step 1 –
Click the link to Medicaid.gov, look to the section I outlined in red.
Step 2 –
Select your state and click on the button they have marked “GO” – it will take you to your State Medicaid Agency with all their contact info.
How to get free neck braces
There are a number of resources which you can use in your state to find out if you can get free neck braces from different state level resources.
I would suggest that looking for free items of equipment like a crutch, or a cane, is somewhat less risky than a neck brace, where your neck may require a very specific brace which has to be diagnosed and fitted by a treating medical practitioner.
That said, the funding sources will pay for a new neck brace etc., but used braces which have been refurbished will need to be properly fitted.
The following are suggestions of where you may find funding for, or free refurbished, neck braces –
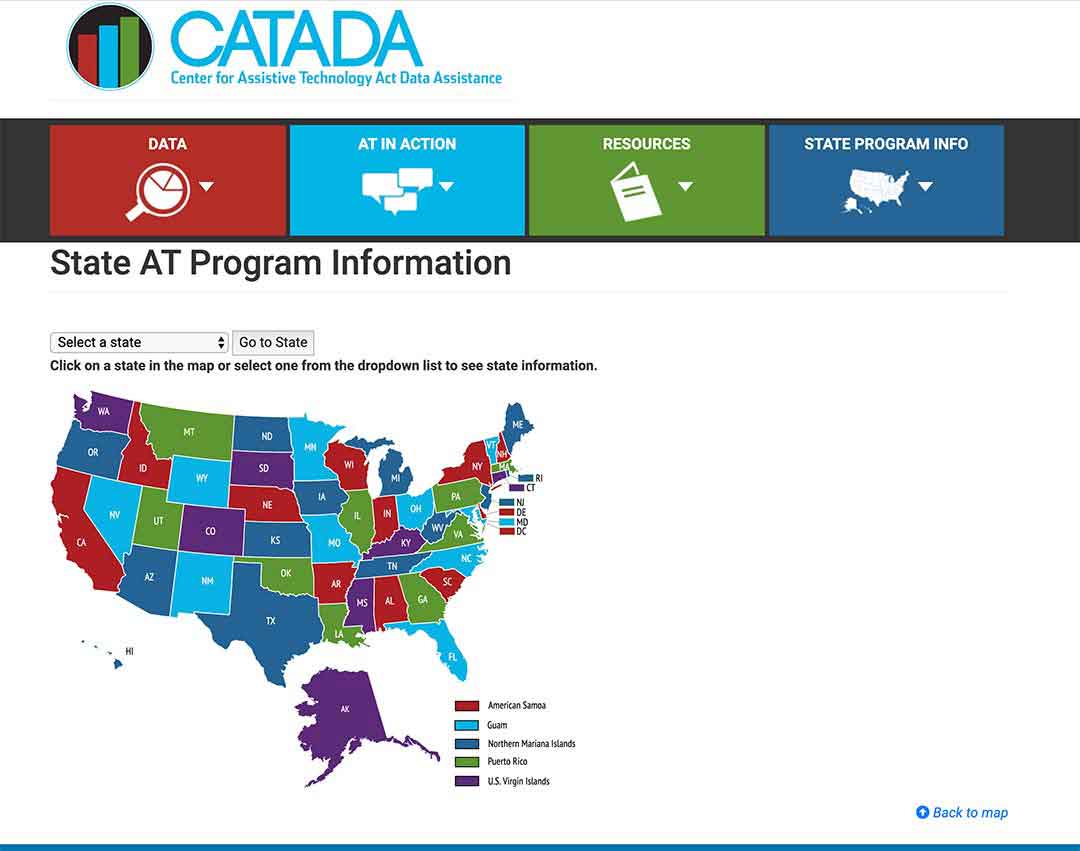
Assistive Technology Programs
Assistive Technology Programs in each state are funded by a national grant to improve access to assistive devices in the home.
The programs concentrate principally on working with the elderly and the disabled.
“Assistive Technology” covers equipment which makes it possible for users to accomplish tasks they otherwise cannot – it can be anything from special shoe horns or adapted stove knobs through to digital safety equipment.
To find out what programs your state runs, click here.
Step 1/
Pick your state on the map or the drop-down menu, and click on “Go to state”
– I chose Florida for this example
Step 2/
Click on the link “Program Title” – for my example, I outlined it in red.
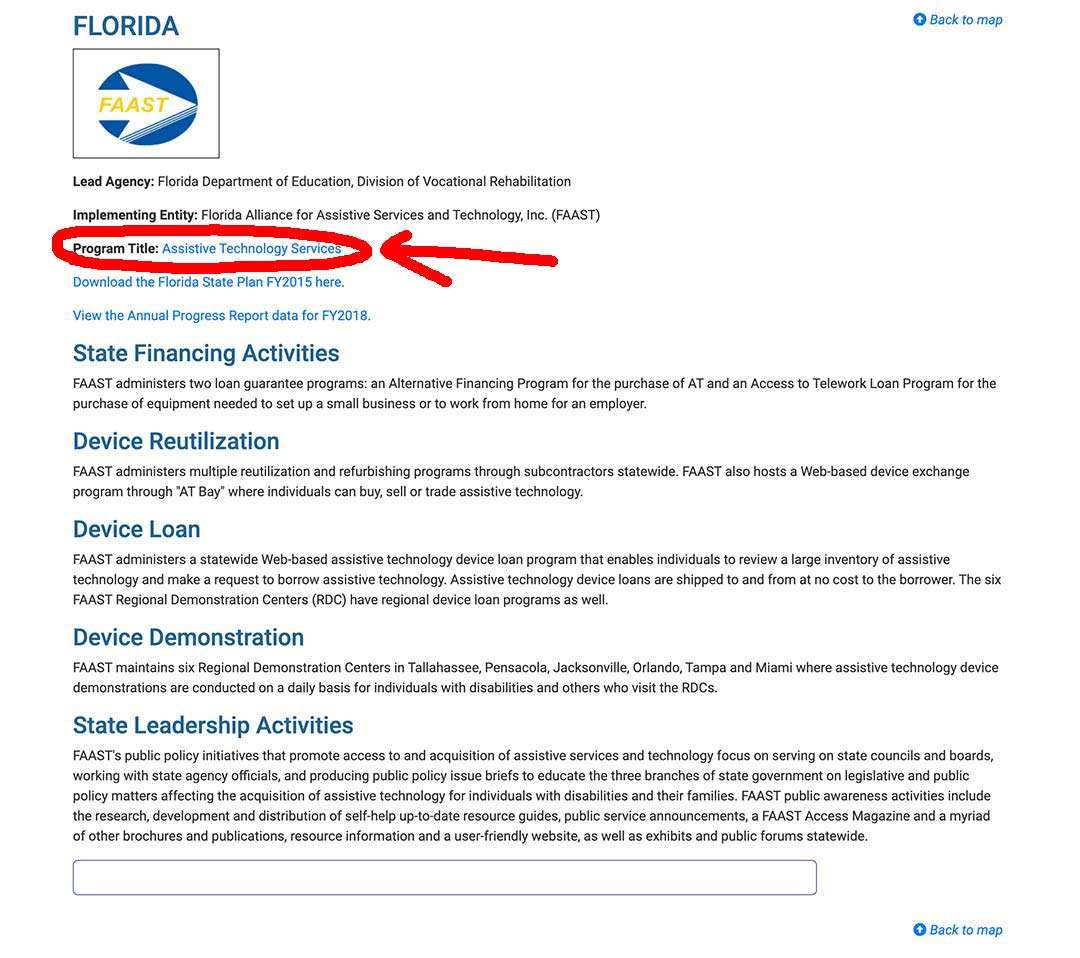
Step 3/
The AT Program state website will come up, and you can sign up, or use their contact info.
State Financial Assistance Programs
State Financial Assistance programs are non-Medicaid programs which help the elderly to remain living as independently as possible in their own homes.
With grants and loans, or a combination of both, the programs will pay for safety equipment, assistive equipment, and sometimes for remodeling homes.
The programs principally focus on the elderly and the disabled.
Your local Area Agency on Aging should be able to help you find out if you have one in your state.
Free neck braces near me ?
The following are ways for finding free medical equipment near to where you live.
Free neck brace on online listings and groups
Here’s a list of online listings where you may be able to find free medical equipment.
The wonderful thing with these online listings and groups, is that you can make the searches as local as you want.
Important points to remember –
- There is going to be no guarantee of the quality of the equipment you are going to find, and if it breaks, and you or someone else, get hurt, you won’t have any recourse, you will be accepting it for free in the condition that you find it
- Go to meetings to pick up equipment with another person – you never know who you are meeting.
- Do not have people deliver to your home – meet up somewhere local away from your home to meet
- Do not give out your personal email – if on Craigslist get a new email just for this, as you may get inundated with spam emails when you sign up to check the listings
List of online listings and groups where you can find used medical equipment –
- Craigslist online listing
- UsedHME.com
- Freecycle.org
- Nextdoor.com
- Facebook Groups and Facebook Marketplace
- Buynothingproject.org
Free neck braces from Medical Equipment loan closets
Medical equipment loan closets are also called –
- medical equipment lending libraries
- community loan closets
- assistive technology lending libraries
- lending libraries
- medical equipment banks
Check to see if your local community administrations know of any in your area. You can contact your town council human services, or senior services department, or any public senior center near you to ask if they know of any.
The loan closets are usually run by volunteers and offer free, gently used, equipment on loan, either temporary or long term.
I have found many loan closets run by American Legion and Lions Clubs, for their local communities, and a few by Elk lodges.
Where to ask about free neck braces in your neighborhood
If you have had no luck with the options so far, you want to contact one, or more, of the following groups in your neighborhood to ask if they know of any group who can help with your search –
- Your local Area Agency on Aging
- Lions Clubs
- Rotary Clubs
- Local church communities
Summary
You can get 80% coverage for rigid and semi-rigid neck braces with Medicare Part B, if you have a signed prescription from a Medicare-enrolled doctor stating that it is “medically necessary“.
The braces can be “Custom Fitted” or “Off-The-Shelf” and your doctor will tell you what type you need, if you qualify for coverage.
Only get your brace through a Medicare-enrolled “Participating” supplier who accepts “assignment” and you will only have to pay a co-payment of 20% and your deductible if it applies.
If you don’t qualify under Medicare, you may be able to qualify with Medicaid. If your income is a little too high, don’t forget to check and see if your state has Spend-Down, and see if you qualify.
You may also be eligible for different state funded programs which help the elderly to maintain their independence, along with Medicaid HCBS programs, waivers and 1915 waivers.
If you are a little overwhelmed by tracking everything down, I would either call your state SHIP program for a chat, or just find out where your local Area Agency on Aging is, and go and see if they can give you help with finding resources.
I’m Gareth, the author and owner of Looking After Mom and Dad.com
I have been a caregiver for over 10 yrs and share all my tips here.

